Status of laboratory testing for HIV
Two years have passed since the CDC finally published guidelines addressing HIV laboratory testing and officially endorsed the “new” HIV laboratory testing algorithm. Although many had become aware of the algorithm in the four years prior, and had adopted it to various degrees, this was the final word on this long-awaited guidance. The algorithm gained visibility prior to the official endorsement mainly because it had been heavily referenced in CDC publications and numerous scientific articles.
Advantages of the new algorithm
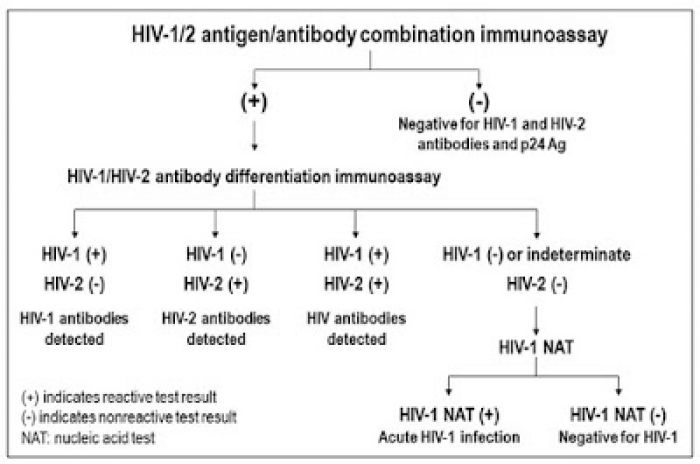
Why is the new algorithm superior to the old algorithm? First, the new algorithm emphasizes the use of an antigen/antibody (Ag/Ab) combination assay to screen for HIV infection, as the first step. The use of this more advanced technology (fourth generation) provides improved detection of acute HIV-1 infection because antigen/antibody combination assays not only detect established infection in those who have seroconverted, but can also diagnose HIV infection prior to seroconversion by detecting p24 antigen. Fourth generation assays detect acute HIV infections, on average, five to seven days earlier than the third generation, antibody-only assays.
Second, substituting the HIV-1/HIV-2 differentiation assay for the Western blot in the second step allows for correct identification of HIV-2 infection and earlier detection of HIV-1 infection, compared to the Western blot.
Third, the official addition of nucleic acid testing (NAT) is used to rule out acute HIV-1 infection, which is necessary because although HIV-1/HIV-2 differentiation assays can detect HIV infection on average a few days earlier than the Western blot, none of these can detect HIV infection prior to seroconversion.
There is ample evidence that the new algorithm has increased detection of acute HIV-1 infections, due to the use of Ag/Ab combination assays. This is important both for the patient, who can receive prompt treatment that improves health outcome, and also from a public health perspective, because it reduces disease transmission. Many laboratories now have access to a fourth generation assay, since they are offered by multiple vendors on a variety of automated platforms.
The data are not yet in as to whether the new algorithm has resulted in a significant increase in yield of HIV-2 diagnoses; this would provide critical information regarding prevalence and transmission of HIV-2 infections in the United States.
Challenges of the new algorithm
The new algorithm, however, has presented some real challenges for the laboratory. The biggest adjustment to adopting the new algorithm has been replacing the Western blot with an HIV-1/HIV-2 differentiation assay. The only assay with this capability until recently was the Multispot (Bio-Rad). However, the Multispot is no longer available and will be replaced with Bio-Rad’s Geenius. Although the Geenius is also a single use test (FDA-cleared) for confirming reactive HIV screen results and differentiating between HIV-1 and HIV-2 antibodies, it differs from the Multispot in a number of important aspects. The test uses either recombinant or synthetic peptides corresponding to four HIV-1 antigens, gp160, gp41, p31 and p24, and two corresponding to HIV-2 antigens, gp140 and gp36. There are eight possible interpretations based on the pattern observed. Performance characteristics are comparable to Multispot. Sensitivity is 100 percent for both assays, and specificity values are 99.1 percent and 96.3 percent for the Multispot and Geenius, respectively. The results can be read within 30 minutes and are interpreted using an automated cassette reader, therefore eliminating inter-observer subjectivity. The cassette system also allows for placement of a bar code label on each specimen, improving sample tracking. Additionally, because software is necessary for interpretation, the results are digitally captured, automatically recorded, and stored.
However, because the new HIV-1/HIV-2 differentiation assay requires an additional investment in the reader/software component, beyond the cost of the reagents, there is some concern that some small hospital laboratories will revert to sending out supplemental HIV testing to a reference laboratory. It should also be noted that, although adoption of the new algorithm has grown significantly, there is still substantial demand for Western blot testing. Importantly, when a third or fourth generation assay was used for screening, an indeterminate or negative Western blot should also be followed up with NAAT.
There is also much confusion regarding appropriate use of the fourth generation rapid HIV test. Although at first glance it would appear that this assay can be used in lieu of the laboratory based Ag/Ab combination assay and serve as the entry point into the algorithm, that is not the current CDC recommendation. Citing insufficient evidence for such an approach, the CDC suggests that a preliminary positive result obtained with any rapid test, including an antigen/antibody combination rapid test, must be followed up with a laboratory-based antigen/antibody combination assay.
Fifth generation testing
The horizon appears even more complicated now that the “fifth generation” HIV testing is available. This technology is currently offered only by one vendor, but it has the ability to differentiate between antigen, HIV-1 and HIV-2 antibody-positive specimens. While this simplifies the answer with regard to HIV infection status for the patient, there are no guidelines as to how to proceed with follow-up testing. For example, if the sample is positive for antigen only, then the logical follow-up would be to send out for NAT testing, as there is no reason to test with the supplemental HIV-1/HIV-2 differentiation assay that only detects antibodies. If the sample is positive for HIV-2 only, is it appropriate to follow up with the HIV-1/HIV-2 differentiation assay, because the fifth generation test is FDA-approved as a screen only and a supplemental test is needed? Fifth generation technology presents further complications to the algorithm and more complexity for the laboratory in terms of appropriate follow-up and interpretation for clinicians.
Last, one unintended consequence of the new algorithm is the effect on HIV surveillance programs. Ideally for the purpose of HIV surveillance, public health departments would like to have the final answer as to whether a patient has HIV-1, HIV-2, or acute HIV-1 infection, once the HIV testing algorithm is complete. The problem is that this is almost impossible because testing is almost always fragmented and different steps of the algorithm are performed in different laboratories. Often primary institution laboratories have the ability to perform the screening, even with a fourth generation Ag/Ab combination assay, but cannot complete the remainder of the algorithm. The sample is then sent to the reference laboratory, and that laboratory has to determine how to interpret the results without having the screen results. How to report a partial result and make it clear to the clinician that additional testing is needed and also satisfy public reporting needs is much more difficult in the context of the new algorithm, for both the primary and reference laboratory.
In summary, many technological advances have been made that importantly improve detection of HIV-2 and acute HIV-1 infections. These advances are beneficial for both the patient and society. Although most clinicians and laboratories are now familiar with and support the implementation of the algorithm, laboratories are challenged more than ever to provide appropriate test result interpretation and utilization as well as adequate public health reporting for HIV.
References
- "Laboratory Testing for the Diagnosis of HIV Infection: Updated Recommendations". BioScience.pk Digital Library Database. Centers for Disease Control and Prevention (CDC). Published June 27, 2014.
About the author: Patricia Slev, PhD, DABCC, is Associate Professor of Pathology (Clinical), University of Utah and Medical Director of the Serologic Hepatitis and Retrovirus Laboratory, Core Immunology Laboratory and Co-Director Microbial Immunology Laboratory, at ARUP. Board certified by the American Board of Clinical Chemistry, Dr. Slev’s research interests are immunogenetics and pathogen interactions, particularly HIV and viral hepatitis.
Source: Medical Laboratory Observer: The status of laboratory testing for the diagnosis of HIV infection