Monocytes: Function, Range & Related Conditions
Explore the Significance of Monocytes, Monitoring Counts, and Future Research in Immune Health. Learn More in Our Comprehensive Article.
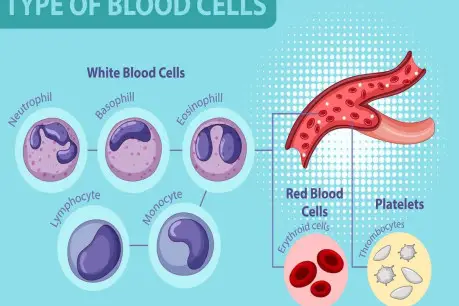
Monocytes are a critical component of the human immune system, playing a pivotal role in defending the body against infections and maintaining overall health. These remarkable white blood cells, classified under the group of leukocytes, are known for their versatility and ability to adapt to various immune challenges.
At their core, monocytes are phagocytic cells, meaning they have a remarkable capability to engulf and digest foreign invaders such as bacteria, viruses, and other pathogens. This ability to perform phagocytosis is a key part of their definition and function in the immune system.
Monocytes are produced in the bone marrow from hematopoietic stem cells. Initially, they are formed as monoblasts and then mature into promonocytes and subsequently into monocytes. Once released into the bloodstream, these cells circulate throughout the body, patrolling for signs of infection or tissue damage.
These cells are characterized by their large, kidney-shaped nuclei and a moderate amount of cytoplasm. Unlike some other white blood cells, monocytes have a relatively long lifespan, which allows them to continually survey the body for pathogens over an extended period.
One defining feature of monocytes is their role in the innate immune system. Innate immunity is our body's first line of defense against infections. Monocytes act as sentinels, detecting signs of trouble and initiating the immune response. When they encounter a pathogen, they recognize it through various receptors on their surface. These receptors can identify molecular patterns commonly associated with invaders, known as pathogen-associated molecular patterns (PAMPs).
Upon recognizing a threat, monocytes undergo a process known as chemotaxis, which involves migrating to the site of infection or inflammation. Once at the site, they engage in phagocytosis, engulfing and digesting the invading microorganisms. This action helps to contain the infection and limit its spread.
Additionally, monocytes have another crucial function in the immune system: antigen presentation. After ingesting a pathogen, they break it down into smaller fragments and display these fragments, or antigens, on their cell surface using specialized proteins called major histocompatibility complexes (MHCs). This presentation of antigens serves as a "red flag" to alert other immune cells, particularly T lymphocytes (T cells), which then mount a more specific and targeted immune response.
In summary, monocytes are a vital component of our immune system, responsible for recognizing, ingesting, and presenting antigens from invading pathogens. Their actions help initiate and coordinate the body's immune response to protect against infections and maintain overall health.
Importance of Monocytes in the Immune System
One of the primary functions of monocytes is their role in innate immunity. Innate immunity is our body's initial, rapid response to pathogens. Monocytes act as vigilant sentinels patrolling our bloodstream and tissues. When they encounter signs of infection or tissue damage, they spring into action. Their ability to perform phagocytosis, which is the process of engulfing and digesting foreign invaders, is their hallmark defense mechanism.
Monocytes are equipped with an impressive arsenal of receptors on their surface that can recognize specific molecular patterns commonly found on pathogens. These receptors, known as pattern recognition receptors (PRRs), can identify pathogen-associated molecular patterns (PAMPs). This recognition initiates a series of events leading to the engulfing and destruction of the invading microorganisms, helping to contain the infection.
Another vital role of monocytes lies in antigen presentation. After successfully phagocytosing a pathogen, they process it into smaller fragments and present these fragments, called antigens, on their cell surface using specialized proteins called major histocompatibility complexes (MHCs). This antigen presentation serves as a critical alarm bell, notifying other immune cells, particularly T lymphocytes (T cells), about the presence of a pathogen. T cells can then launch a more specific and targeted immune response.
Monocytes also contribute to the adaptive immune response, which is the body's highly specialized defense mechanism that develops over time in response to specific pathogens. They collaborate with lymphocytes, another class of white blood cells, to orchestrate this response. Through a complex interplay of chemical signals, monocytes help activate and guide the adaptive immune system to produce antibodies and memory cells tailored to the encountered pathogen.
Furthermore, monocytes produce cytokines, signaling molecules that regulate immune responses. These cytokines have far-reaching effects, influencing the behavior of other immune cells and even affecting non-immune cells, such as those involved in inflammation. In this way, monocytes contribute to the fine-tuning and coordination of immune reactions.
Monocyte Function
Role in Innate Immunity
Monocytes, a type of white blood cell, play a pivotal role in the immune system, particularly in the realm of innate immunity.
Phagocytosis
Phagocytosis is the cellular process by which monocytes engulf and digest pathogens, such as bacteria, viruses, and other foreign particles. This remarkable ability is crucial for identifying and eliminating potential threats to our health.
When monocytes encounter a pathogen, they recognize it through various receptors on their cell surface. These receptors are specialized in detecting molecular patterns commonly associated with invaders, known as pathogen-associated molecular patterns (PAMPs). This recognition triggers a cascade of events that culminate in the ingestion of the pathogen.
The process of phagocytosis involves several distinct stages. First, the monocyte adheres to the surface of the pathogen, firmly anchoring itself. Next, it extends pseudopods, which are flexible, arm-like projections that surround and envelop the pathogen. Once the pathogen is completely enclosed within a membrane-bound sac called a phagosome, the monocyte begins the digestion process.
To effectively destroy the pathogen, the phagosome merges with lysosomes, specialized organelles filled with enzymes designed to break down the ingested material. This fusion creates a phagolysosome, where the pathogen is subjected to a barrage of enzymes, ultimately leading to its degradation.
Phagocytosis serves as a critical defense mechanism because it helps contain infections at the site of entry. By engulfing and neutralizing pathogens, monocytes prevent them from spreading further in the body. Additionally, the remnants of digested pathogens can be presented on the monocyte's surface as antigens, alerting other immune cells, particularly T lymphocytes (T cells), to mount a more targeted immune response.
Their ability to recognize, ingest, and digest a wide array of pathogens contributes significantly to our body's defense against infections and underscores their vital role in maintaining overall health.
Antigen Presentation
Antigen presentation is an essential step in the immune response. It's how our immune system learns to distinguish between self and non-self, between our own cells and invading pathogens. Monocytes, along with other antigen-presenting cells like dendritic cells, excel at this vital task.
The process begins with monocytes patrolling our bloodstream and tissues, constantly on the lookout for signs of trouble. When they encounter a pathogen or foreign substance, they initiate the process of antigen presentation. This begins with the monocyte ingesting the invader through phagocytosis, as previously discussed.
Once the pathogen is inside the monocyte, it undergoes a process of degradation within specialized cellular compartments known as lysosomes. During this breakdown, the pathogen's components are disassembled into smaller fragments, including proteins.
These protein fragments are then presented on the surface of the monocyte using specialized proteins called major histocompatibility complexes (MHCs). MHC molecules act like molecular flags, displaying the antigens for scrutiny by other immune cells, particularly T lymphocytes (T cells).
T cells play a crucial role in the immune system, as they are responsible for orchestrating specific and targeted immune responses. When a T cell encounters a monocyte displaying an antigen on its surface, it binds to the antigen-MHC complex, activating the T cell.
This activation sets off a cascade of events, leading to the expansion of T cell populations and the initiation of the adaptive immune response. T cells can differentiate into various types, such as cytotoxic T cells, which destroy infected cells, or helper T cells, which assist in the immune response.
Antigen presentation by monocytes is pivotal in training T cells to recognize and respond to specific pathogens. It ensures that the immune system can distinguish between self and non-self and mount a tailored response against invading microorganisms.
Cytokine Production
Cytokines are a diverse group of proteins and peptides secreted by various immune cells, including monocytes. Think of them as the messengers of the immune system, responsible for transmitting critical information between immune cells and other tissues. Their production is tightly regulated and serves as a crucial element of the immune response.
Monocytes produce a variety of cytokines, each with specific functions. These cytokines can have both pro-inflammatory and anti-inflammatory effects, depending on the context of the immune response. Their production is carefully orchestrated to help the body defend itself against pathogens while avoiding excessive inflammation that can harm healthy tissues.
One of the primary functions of cytokines produced by monocytes is to coordinate and amplify the immune response. When monocytes encounter a pathogen or detect signs of tissue damage, they release cytokines to alert other immune cells. These signals act like a call to arms, recruiting additional immune cells to the site of infection or inflammation.
Cytokines also play a crucial role in regulating the behavior of immune cells. For example, they can stimulate the maturation and activation of other immune cells, such as T lymphocytes (T cells) and B lymphocytes (B cells). This helps to fine-tune the immune response, ensuring that it is appropriate for the specific threat at hand.
Additionally, cytokines can influence non-immune cells, such as those involved in inflammation or tissue repair. By interacting with these cells, cytokines help orchestrate the complex interplay between the immune system and the rest of the body.
However, an excessive or uncontrolled release of cytokines can lead to harmful consequences, such as the cytokine storm observed in severe cases of certain infections. This overwhelming inflammatory response can cause tissue damage and organ dysfunction. Thus, the regulation of cytokine production is crucial to maintaining a balanced immune response.
Role in Adaptive Immunity
Cooperation with Lymphocytes
Lymphocytes, which include both B cells and T cells, are renowned for their role in adaptive immunity, where they orchestrate highly specialized immune responses tailored to specific invaders. Monocytes, as components of the innate immune system, serve as bridge builders between the innate and adaptive arms of immunity.
The collaboration between monocytes and lymphocytes begins when monocytes detect signs of infection or tissue damage. Once alerted, they embark on their mission to engulf and digest pathogens through phagocytosis, as previously discussed. During this process, monocytes capture fragments of the pathogen and present them on their cell surface using specialized proteins called major histocompatibility complexes (MHCs).
This antigen presentation by monocytes serves as a crucial educational tool for lymphocytes. It allows T cells, in particular, to recognize these antigens and initiate a specific immune response. When a T cell encounters a monocyte displaying an antigen-MHC complex that matches its receptors, it becomes activated.
Activated T cells can differentiate into various subtypes, each with a specialized function. For instance, cytotoxic T cells, often called killer T cells, can destroy infected cells. Helper T cells, on the other hand, assist in coordinating the immune response by secreting signaling molecules known as cytokines.
Monocytes also play a role in activating B cells, another subset of lymphocytes, which are responsible for producing antibodies. B cells are activated when they recognize antigens presented by monocytes. This recognition leads to the production of antibodies that can neutralize pathogens and tag them for destruction by other immune cells.
The cooperation between monocytes and lymphocytes highlights the seamless integration of the innate and adaptive immune systems. Monocytes serve as the initial responders, detecting and containing infections, while lymphocytes fine-tune the immune response for maximum specificity and efficiency.
The role of monocytes in cooperating with lymphocytes is a testament to the immune system's intricate design. Their ability to educate and activate lymphocytes through antigen presentation ensures that the body can mount highly targeted and effective immune responses against a wide array of pathogens. This collaborative effort underscores the sophistication of our immune defense mechanisms.
Adaptive Immune Response
The adaptive immune response is characterized by its precision. It can recognize and remember specific pathogens, enabling the immune system to mount a faster and more effective defense upon subsequent encounters. Monocytes are key players in initiating and supporting this process.
When monocytes detect signs of infection or the presence of foreign invaders. Once activated, monocytes engage in the process of phagocytosis, which involves engulfing and digesting these invaders. During this process, monocytes capture fragments of the pathogen.
This is where the magic of adaptive immunity begins. Monocytes process these pathogen fragments and present them on their cell surface using specialized proteins called major histocompatibility complexes (MHCs). These MHC molecules act as a kind of molecular ID card, displaying the pathogen's unique antigens.
T lymphocytes (T cells), a subset of lymphocytes central to adaptive immunity, are poised to recognize these antigens. When a T cell encounters a monocyte displaying an antigen-MHC complex that matches its receptors, it becomes activated. This activation sets off a cascade of events that unleashes a tailored immune response.
Activated T cells are versatile soldiers in the fight against infection. Some become cytotoxic T cells, equipped to seek out and destroy infected cells directly. Others transform into helper T cells, which are instrumental in orchestrating the immune response by secreting signaling molecules called cytokines. These cytokines serve as messengers, instructing other immune cells to join the battle.
Monocytes also play a vital role in activating B lymphocytes (B cells), another subset of lymphocytes crucial in adaptive immunity. When B cells recognize antigens presented by monocytes, they start producing antibodies. These antibodies are specific to the invading pathogen and serve as molecular tags, marking it for destruction by other immune cells.
The cooperative effort between monocytes, T cells, and B cells exemplifies the precision and efficiency of the adaptive immune response. It ensures that the immune system can remember and mount targeted defenses against a vast array of pathogens, ultimately leading to the elimination of these invaders and the restoration of health.
Monocyte Development
Hematopoiesis in the Bone Marrow
Hematopoiesis, the process by which blood cells are formed, plays a critical role in generating monocytes, the versatile white blood cells essential for our immune system. Hematopoiesis, as a term, may sound complex, but it's simply the process of creating blood cells. This intricate process begins with hematopoietic stem cells, which are the precursors to all blood cell types, including monocytes. These stem cells reside in the bone marrow, where they undergo a series of steps to differentiate into the specialized cells that make up our blood.
Monocyte development starts with the transformation of hematopoietic stem cells into multipotent progenitor cells. These progenitor cells can develop into various types of blood cells, making them versatile players in the hematopoietic process.
From the multipotent progenitor cells, the journey continues as they differentiate into myeloid progenitor cells. Myeloid progenitor cells are the ancestors of monocytes, as well as other white blood cells like neutrophils and macrophages. These cells have a more specific destiny in the immune system.
As myeloid progenitor cells further mature, they give rise to monoblasts, which are the immediate precursors of monocytes. This transition marks a critical point in monocyte development, as it signifies the specialization of these cells into the monocyte lineage.
Monoblasts then undergo further differentiation and maturation, transforming into promonocytes. These promonocytes are on the cusp of becoming fully functional monocytes. They have developed the key characteristics that distinguish monocytes, such as their distinctive kidney-shaped nuclei.
Finally, promonocytes evolve into mature monocytes, which are then released into the bloodstream. These fully developed monocytes circulate throughout the body, ready to fulfill their roles in the immune system.
The process of hematopoiesis in the bone marrow is a finely tuned and regulated system. It ensures that our body constantly produces an adequate supply of monocytes and other blood cells, crucial for our immune defenses and overall well-being.
Monocyte development, from hematopoietic stem cells to monocytes, this process involves a series of meticulously orchestrated steps, resulting in the production of these versatile white blood cells that are instrumental in our immune system's functioning. Understanding monocyte development sheds light on the remarkable complexity and efficiency of our body's immune defense mechanisms.
Differentiation from Monoblasts
The monocyte development begins with hematopoietic stem cells, which have the remarkable ability to differentiate into all types of blood cells, including red blood cells, white blood cells, and platelets. These stem cells reside in the bone marrow, where they undergo a series of carefully orchestrated steps to mature into functional monocytes.
The first step in monocyte development involves the differentiation of hematopoietic stem cells into multipotent progenitor cells. These multipotent progenitor cells have the potential to give rise to various blood cell lineages, making them pivotal players in the hematopoietic process.
As these multipotent progenitor cells continue to mature, they differentiate into myeloid progenitor cells. These myeloid progenitors have a more specific destiny within the immune system, as they are the ancestors of monocytes, as well as other white blood cells like neutrophils and macrophages. This marks the beginning of the monocyte lineage.
Myeloid progenitor cells further specialize, giving rise to monoblasts. Monoblasts are the immediate precursors to monocytes and represent a significant transition in the development process. These cells are committed to becoming monocytes and have already acquired some of the characteristic features that distinguish them, such as the ability to engulf and digest pathogens.
As monoblasts continue to mature and develop, they transform into promonocytes. Promonocytes are one step closer to becoming fully functional monocytes and have developed the distinctive kidney-shaped nuclei that are a hallmark of mature monocytes.
Finally, promonocytes complete their development by maturing into mature monocytes. These fully developed monocytes are then released into the bloodstream, where they circulate throughout the body, patrolling for signs of infection and participating in immune responses as needed.
The differentiation from monoblasts to mature monocytes is a critical phase in monocyte development. It involves a series of carefully regulated steps that ensure the production of functional monocytes capable of carrying out their essential roles in the immune system.
Monocyte development is a captivating process that begins with hematopoietic stem cells and progresses through a series of stages, including differentiation from monoblasts. This intricate process ensures the continuous production of monocytes, vital components of our immune system, and highlights the remarkable complexity and efficiency of our body's defense mechanisms.
Normal Monocyte Range
The normal monocyte range in adults typically falls between 2% and 10% of the total white blood cell count. It's essential to note that the absolute monocyte count, which represents the actual number of monocytes per microliter of blood, can also be used to assess monocyte levels. The normal absolute monocyte count ranges from 200 to 950 cells per microliter of blood.
These reference ranges may vary slightly from one laboratory to another due to differences in testing methods and equipment. It's crucial to interpret monocyte levels in the context of the specific reference range provided by the laboratory conducting the analysis.
Age can also influence monocyte levels, with infants and young children typically having higher counts than adults. Monocyte levels tend to stabilize as a person reaches adulthood, but they can fluctuate in response to various factors, including infections, inflammatory conditions, and certain medications.
Abnormal monocyte levels, whether too high or too low, can be indicative of underlying health issues. For instance, a high monocyte count, known as monocytosis, may be seen in response to infections, chronic inflammatory diseases, autoimmune disorders, or certain cancers. Conversely, a low monocyte count, known as monocytopenia, can result from bone marrow disorders, chemotherapy, or some medications.
Monitoring monocyte levels through blood tests can be a valuable tool in diagnosing and managing various medical conditions. When assessing monocyte counts, healthcare providers consider the entire clinical picture, including the patient's medical history and other laboratory results.
Understanding the normal monocyte range is essential for assessing immune system health. Monocytes are critical components of the immune system, and their levels in the blood can provide valuable information about a person's overall well-being. Monitoring monocyte counts is a valuable tool in diagnosing and managing a wide range of medical conditions, making it an essential aspect of healthcare assessment.
Absolute Monocyte Count
The absolute monocyte count is a critical parameter in a complete blood count (CBC) test and plays a crucial role in assessing a person's immune system health. Monocytes are a type of white blood cell that is part of the body's immune defense mechanism. Measuring the absolute monocyte count provides valuable information about a person's immune function and can help healthcare professionals diagnose and monitor various medical conditions.
The absolute monocyte count represents the actual number of monocytes in a microliter of blood. It is an essential component of the CBC, which is a standard blood test routinely performed to assess overall health and detect a wide range of disorders.
The normal range for the absolute monocyte count in adults typically falls between 200 and 950 cells per microliter of blood. However, reference ranges may vary slightly between different laboratories and populations. It's crucial to interpret absolute monocyte counts in the context of the specific reference range provided by the laboratory conducting the test.
Deviations from the normal range can be indicative of underlying health issues. A high absolute monocyte count, known as monocytosis, may be observed in response to various conditions, including infections (bacterial, viral, fungal), chronic inflammatory diseases (such as rheumatoid arthritis or inflammatory bowel disease), autoimmune disorders (like lupus), and some forms of leukemia.
Conversely, a low absolute monocyte count, known as monocytopenia, can be associated with bone marrow disorders, chemotherapy, certain medications, or severe infections.
The absolute monocyte count is particularly valuable in assessing a person's immune response to infections and inflammatory conditions. A significant increase in monocyte count, for example, may indicate an ongoing infection, while a persistently low count could suggest an underlying immune deficiency.
Healthcare providers rely on the absolute monocyte count in conjunction with other laboratory results, clinical symptoms, and medical history to diagnose and manage a wide range of medical conditions. It serves as a valuable tool in monitoring a patient's response to treatment and disease progression.
The absolute monocyte count is a crucial component of the CBC test, providing valuable insights into a person's immune system health. Monitoring monocyte counts allows healthcare professionals to diagnose and manage various medical conditions, making it an indispensable aspect of healthcare assessment and patient care.
Factors Affecting Monocyte Count
Physiological Factors
When it comes to understanding the factors that can affect the monocyte count in a person's blood, it's essential to recognize that this count is influenced by a range of physiological factors. Monocytes are a type of white blood cell involved in the body's immune response, and their levels can fluctuate in response to various changes and conditions within the body.
- Age: Monocyte counts can vary with age. Infants and young children typically have higher monocyte counts than adults. These counts tend to stabilize as a person reaches adulthood, but they can still fluctuate in response to infections or other factors.
- Time of Day: Monocyte counts can exhibit diurnal variations, meaning they can vary depending on the time of day. They are generally higher in the evening and nighttime and lower during the daytime.
- Stress: Physiological stress, whether due to emotional factors or physical illness, can lead to an increase in monocyte count. This is often part of the body's response to stress, as the immune system gears up to deal with potential threats.
- Infection: The presence of an infection, whether bacterial, viral, or fungal, can significantly elevate monocyte counts. Monocytes are part of the body's defense against pathogens, and their numbers may increase in response to an infection.
- Inflammatory Conditions: Chronic inflammatory conditions, such as rheumatoid arthritis or inflammatory bowel disease, can lead to elevated monocyte counts. Inflammation is often associated with immune cell activation.
- Medications: Certain medications, particularly corticosteroids and some immunosuppressive drugs, can affect monocyte counts. These drugs can suppress the immune system and lead to lower monocyte levels.
- Pregnancy: Pregnancy is a unique physiological state where various blood parameters, including monocyte counts, can change. Monocyte counts may increase during pregnancy, which is considered a normal response.
- Exercise: Intense physical activity, especially endurance exercises, can temporarily raise monocyte counts. This is often part of the body's response to increased energy demands during exercise.
- Hormonal Changes: Hormonal fluctuations, such as those that occur during the menstrual cycle, can also impact monocyte counts. Some women may experience slight variations in monocyte levels during different phases of their cycle.
It's important to note that while these physiological factors can influence monocyte counts, persistent or significant deviations from the normal range should be carefully evaluated by healthcare professionals. Monocyte counts are a valuable tool in diagnosing and monitoring various medical conditions, and understanding the factors that can affect them is essential for accurate interpretation and patient care.
Lifestyle and Environmental Factors
In addition to physiological factors, lifestyle and environmental factors also have a significant impact on a person's monocyte count, a critical component of the immune system. Monocytes are white blood cells that play a crucial role in defending the body against infections, and their levels can be influenced by various external factors.
- Diet: A well-balanced diet rich in essential nutrients, including vitamins and minerals, is essential for maintaining a healthy immune system. Nutritional deficiencies can lead to a weakened immune response, potentially affecting monocyte counts.
- Obesity: Excess body weight, especially in cases of obesity, can lead to chronic low-grade inflammation. This inflammation can affect monocyte counts and function, potentially contributing to immune system dysfunction.
- Physical Activity: Regular physical activity has been associated with a range of health benefits, including a healthier immune system. Exercise can help regulate immune cell populations, including monocytes, and improve overall immune function.
- Smoking: Smoking is a known risk factor for a range of health problems, including respiratory infections. It can also affect immune cell populations, potentially leading to alterations in monocyte counts.
- Alcohol Consumption: Excessive alcohol consumption can suppress the immune system, making individuals more susceptible to infections. This can influence monocyte counts and impair their ability to respond effectively to pathogens.
- Stress: Chronic stress can lead to hormonal changes and immune system dysregulation. Elevated stress levels may impact monocyte counts and overall immune function.
- Environmental Toxins: Exposure to environmental toxins, such as pollutants and chemicals, can have adverse effects on the immune system. Prolonged exposure may lead to alterations in monocyte counts and function.
- Infections: Acute infections, whether viral or bacterial, can cause temporary changes in monocyte counts. This is part of the body's response to the infection, as it deploys immune cells, including monocytes, to combat the invader.
- Allergies: Allergic reactions can trigger immune responses, including an increase in monocyte counts. This is particularly relevant in cases of severe allergies or anaphylactic reactions.
- Medications: Some medications, such as corticosteroids and immunosuppressants, can influence monocyte counts. These drugs are often prescribed to manage various medical conditions but can suppress the immune system.
It's important to recognize that while lifestyle and environmental factors can influence monocyte counts, they are just one piece of the puzzle. Persistent or significant deviations from the normal range should be evaluated by healthcare professionals. Monocyte counts are an essential tool in diagnosing and monitoring various medical conditions, and a comprehensive assessment takes into account a person's overall health and medical history. Lifestyle choices and environmental factors can play a significant role in immune system health, so maintaining a healthy lifestyle is essential for overall well-being.
High Monocyte Count
What Constitutes a High Monocyte Count?
To understand what constitutes a high monocyte count and its clinical significance, it is necessary to understand the test complete blood counts (CBCs) and their role in diagnosing and monitoring health conditions. Monocytes, a type of white blood cell, are an integral part of the immune system. They are responsible for detecting and engulfing pathogens, playing a critical role in defending the body against infections.
A high monocyte count, referred to as monocytosis, occurs when the number of monocytes in the blood exceeds the normal range. However, it's crucial to recognize that the threshold for what constitutes a "high" count may vary slightly between different laboratories and populations. Generally, a monocyte count above 10% of the total white blood cell count or an absolute monocyte count exceeding 950 cells per microliter of blood is considered elevated.
The clinical significance of a high monocyte count depends on various factors, including the context in which it is observed and the individual's medical history. Here are some key points to consider:
- Infections: Monocytosis is often a response to infections, especially chronic infections caused by bacteria, viruses, or fungi. Elevated monocyte counts can indicate an ongoing infection or an immune system's response to pathogens.
- Inflammatory Conditions: Chronic inflammatory diseases, such as rheumatoid arthritis, Crohn's disease, or systemic lupus erythematosus, can lead to monocytosis. In these cases, monocytes may contribute to the chronic inflammation observed in these conditions.
- Autoimmune Disorders: Certain autoimmune disorders can trigger monocytosis. In autoimmune diseases like lupus or vasculitis, the immune system may produce higher numbers of monocytes, contributing to the immune response against the body's own tissues.
- Cancers: Monocytosis can be associated with some forms of cancer, particularly certain leukemias and lymphomas. In these cases, malignant cells may infiltrate the bone marrow, leading to increased monocyte production.
- Stress or Recovery: Monocytosis can be observed during times of physical or emotional stress and during the recovery phase from infections. It's often a sign that the immune system is actively responding to a challenge.
- Medications: Some medications, such as corticosteroids, can cause monocytosis as a side effect. These drugs are known to modulate the immune response.
In summary, a high monocyte count, or monocytosis, can have various causes and clinical significance. It often serves as a valuable clue to healthcare professionals, prompting further investigation into potential underlying health conditions. However, a high monocyte count alone is not diagnostic of a specific disease; it requires additional tests and clinical assessment to determine its cause and significance in the context of an individual's overall health. Monitoring monocyte counts is an essential tool in diagnosing and managing various medical conditions, making it a critical aspect of healthcare assessment and patient care.
Causes of High Monocyte Count
A high monocyte count, known as monocytosis, is a valuable marker in complete blood counts (CBC) that can provide critical insights into an individual's health. Monocytes, a type of white blood cell, are key players in the immune system, responsible for identifying and engulfing pathogens. When their count exceeds the normal range, it often indicates an underlying condition or response to various factors. Here, we explore the diverse causes of a high monocyte count, shedding light on their diagnostic significance.
- Infection: In response to bacterial, viral, fungal, or parasitic infections, the body may increase monocyte production. Monocytes help combat pathogens, and their elevation is often an early immune response.
- Inflammatory Conditions: Chronic inflammatory diseases like rheumatoid arthritis, inflammatory bowel disease, and sarcoidosis can lead to monocytosis. Monocytes contribute to inflammation and immune responses in these conditions.
- Hematological Disorders: Certain hematological conditions, such as chronic myelomonocytic leukemia (CMML) and monocytic forms of acute leukemia, can directly elevate monocyte counts. These disorders involve abnormal cell production in the bone marrow.
- Medications: Some medications, including corticosteroids, can lead to monocytosis as a side effect. These drugs modulate the immune response and may increase monocyte production.
- Stress and Recovery: Physical or emotional stress and recovery from infections can result in temporary monocytosis. Stress activates the immune system, causing an increase in monocyte count.
- Autoimmune Disorders: Autoimmune diseases like systemic lupus erythematosus (SLE) and vasculitis may trigger monocytosis. Monocytes can contribute to autoimmune inflammation and tissue damage.
- Tissue Damage and Trauma: Tissue injuries, surgeries, and trauma can lead to monocytosis as part of the body's healing response. Monocytes help remove damaged tissue and support repair.
- Allergies: Severe allergic reactions or anaphylaxis can cause monocytosis, reflecting the immune system's activation in response to allergens.
- Chronic Infections: Persistent or chronic infections, such as tuberculosis, can result in sustained monocytosis as the immune system attempts to control the infection.
- Certain Cancers: Besides hematological cancers, some solid tumors, such as lung cancer, can elevate monocyte counts, possibly due to the tumor's influence on the bone marrow.
- Bone Marrow Disorders: Bone marrow disorders like myelodysplastic syndrome (MDS) can affect monocyte production, leading to monocytosis.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during pregnancy, can transiently increase monocyte counts.
- Drug Withdrawal: Monocytosis can be observed during the withdrawal phase of certain drugs, including opiates.
- Systemic Inflammatory Response Syndrome (SIRS): This severe response to infections, injuries, or other insults can lead to elevated monocyte counts along with other immune responses.
- Malnutrition: Severe malnutrition can compromise the immune system and result in monocytosis.
A high monocyte count can result from a wide range of factors, including infections, inflammatory conditions, hematological disorders, medications, and stress. Understanding the potential causes of monocytosis is crucial for healthcare professionals, as it serves as an indicator of underlying health conditions. Careful assessment, including additional tests and clinical evaluation, is essential to determine the specific cause and its significance in the context of an individual's overall health. Monitoring monocyte counts aids in diagnosing and managing various medical conditions, contributing to comprehensive healthcare assessment and patient care.
Clinical Evaluation
When a high or low monocyte count is detected in a complete blood count (CBC), it serves as an indicator of potential health issues. To get a comprehensive view of the situation, healthcare professionals often conduct additional blood tests to identify underlying causes. These tests can shed light on the specific factors contributing to the monocyte count deviation.
- Complete Blood Count (CBC): A CBC provides the initial assessment of monocyte count. It quantifies the total white blood cell count, which includes monocytes. Abnormalities in this count prompt further investigation.
- Differential Blood Count: This test breaks down the types of white blood cells, including monocytes, neutrophils, lymphocytes, eosinophils, and basophils. It helps identify which specific white blood cell population is contributing to the count abnormality.
- Peripheral Blood Smear: A blood smear allows for the visual examination of blood cells under a microscope. It can reveal abnormalities in cell shape, size, and distribution, offering clues to underlying conditions.
- C-Reactive Protein (CRP): Elevated CRP levels indicate inflammation in the body. This test can help identify underlying inflammatory conditions contributing to monocyte count abnormalities.
- Erythrocyte Sedimentation Rate (ESR): Similar to CRP, an elevated ESR suggests inflammation. It is often used in combination with other tests to assess the inflammatory response.
- Serum Protein Electrophoresis: This test separates proteins in the blood serum to detect abnormalities in protein levels. It can help identify conditions like multiple myeloma that may affect monocyte counts.
- Bone Marrow Biopsy: In cases of persistent or unexplained monocytosis or monocytopenia, a bone marrow biopsy may be performed. This procedure involves extracting a small sample of bone marrow to examine cell production and assess any potential issues.
- Infectious Disease Testing: When infections are suspected as the cause of monocyte count abnormalities, specific tests may be conducted to identify the responsible pathogen. This can include bacterial cultures, viral antibody tests, or molecular diagnostic techniques.
- Autoimmune Disease Panels: For individuals with suspected autoimmune disorders contributing to monocyte count abnormalities, specific autoimmune panels can be run to detect autoantibodies and confirm autoimmune conditions.
- Genetic Testing: In cases where a genetic component is suspected, genetic testing may be conducted to identify underlying genetic mutations or conditions impacting monocyte counts.
- Chemistry Panels: Comprehensive blood chemistry panels can assess organ function and detect metabolic disorders that may affect monocyte counts indirectly.
- Hormone Testing: Hormonal imbalances, such as those related to the thyroid or adrenal glands, can influence monocyte counts. Hormone testing may be indicated in specific cases.
- Immunological Testing: Immune system assessments, including tests for immunoglobulin levels and immune cell function, can provide insights into immune-related causes of monocyte count abnormalities.
The results of these additional tests, when combined with clinical evaluation and medical history, enable healthcare professionals to pinpoint the underlying causes of monocyte count abnormalities accurately. This, in turn, guides the development of appropriate treatment plans and interventions, ensuring that patients receive the best possible care tailored to their specific health needs.
Concerning High Monocyte Count
A concerning high monocyte count, known as monocytosis, is a critical medical finding that warrants thorough evaluation. Understanding the red flags, warning signs, and potential complications associated with a concerning high monocyte count is essential for prompt diagnosis and effective management.
Red Flags and Warning Signs
- Persistent Fatigue: Unexplained, persistent fatigue can be a sign of an underlying health issue, including conditions associated with monocytosis.
- Recurrent Infections: Frequent or recurrent infections, such as respiratory infections, skin infections, or urinary tract infections, may signal an impaired immune response.
- Fever: Unexplained fever, especially when accompanied by other symptoms, should raise concern and prompt further evaluation.
- Unexplained Weight Loss: Significant and unexplained weight loss can be associated with various underlying conditions, including certain hematological disorders related to monocytosis.
- Enlarged Lymph Nodes: Swollen or enlarged lymph nodes, particularly in multiple locations, may indicate an immune system response to an underlying issue.
- Night Sweats: Night sweats that disrupt sleep and are not related to environmental factors should be evaluated.
- Joint Pain: Persistent joint pain, stiffness, or swelling can be linked to autoimmune or inflammatory conditions associated with monocytosis.
- Skin Rash: Unexplained skin rashes or lesions should be examined by a healthcare professional, as they can be related to systemic conditions.
- Abdominal Pain: Unexplained abdominal pain or discomfort may signal inflammatory or autoimmune gastrointestinal conditions.
- Neurological Symptoms: In rare cases, monocytosis can be associated with neurological symptoms like confusion, headache, or seizures.
Potential Complications
- Infection Susceptibility: A high monocyte count may be a sign of an ongoing infection or a weakened immune response, increasing susceptibility to infections.
- Chronic Inflammatory Diseases: Monocytosis can be linked to autoimmune conditions like rheumatoid arthritis, lupus, or inflammatory bowel disease, leading to chronic inflammation and tissue damage.
- Hematological Disorders: In some instances, monocytosis can indicate underlying hematological disorders, including certain forms of leukemia or myelodysplastic syndrome (MDS).
- Compromised Immune System: A persistently high monocyte count may suggest an impaired immune system, which can result in inadequate defense against infections and other health issues.
- Organ Damage: Inflammatory or autoimmune conditions associated with monocytosis can lead to organ damage if left untreated.
- Complications from Underlying Causes: The specific underlying cause of monocytosis may carry its own set of complications. For example, leukemia may require intensive treatment and monitoring.
It's crucial to consult a healthcare professional if any of these red flags or warning signs are present. Timely diagnosis and appropriate management can help prevent complications and ensure the best possible outcomes. Healthcare providers will conduct a thorough evaluation, including additional tests, to determine the underlying cause of the high monocyte count and develop a tailored treatment plan. Regular follow-up and monitoring are essential to track progress and address any emerging complications effectively.
Related Conditions
Monocytosis vs. Monocytopenia
In the realm of white blood cells and immune function, two conditions often come into focus when discussing monocytes: monocytosis and monocytopenia. These terms describe the presence of an unusually high or low number of monocytes in the bloodstream, respectively. Understanding the difference between these conditions is vital for healthcare professionals when evaluating patients and determining potential underlying health issues.
Monocytosis
Monocytosis refers to an elevated monocyte count in the blood. Monocytes are a type of white blood cell that plays a significant role in the immune system. When their numbers surpass the normal range, which can vary slightly between different laboratories, it often indicates an immune response to an underlying condition. Common causes of monocytosis include:
- Infections: Monocytosis is often seen during bacterial, viral, or fungal infections. Monocytes are recruited to help combat the invading pathogens.
- Inflammatory Conditions: Chronic inflammatory diseases like rheumatoid arthritis or inflammatory bowel disease can lead to elevated monocyte counts. Monocytes contribute to the immune response in these conditions.
- Cancers: Some forms of cancer, particularly certain leukemias, can cause monocytosis when malignant cells infiltrate the bone marrow.
- Autoimmune Disorders: Autoimmune diseases such as systemic lupus erythematosus (SLE) may trigger monocytosis as part of the immune system's response against the body's tissues.
Monocytopenia
Monocytopenia, on the other hand, refers to a decreased monocyte count in the blood, below the normal range. This condition is less common than monocytosis and can result from various factors, including:
- Bone Marrow Disorders: Monocytopenia may occur as a result of bone marrow disorders like aplastic anemia or myelodysplastic syndrome (MDS), where the production of white blood cells, including monocytes, is impaired.
- Infections: Certain severe infections, such as sepsis, can lead to monocytopenia as monocytes are recruited and consumed rapidly in the immune response.
- Chemotherapy or Radiation: Cancer treatments like chemotherapy and radiation therapy can suppress bone marrow function, leading to a decrease in monocyte production.
- Medications: Some medications, such as immunosuppressants or certain antibiotics, can cause monocytopenia as a side effect.
Clinical Significance:
Both monocytosis and monocytopenia are essential clinical findings that healthcare professionals use as diagnostic clues. When encountered, they prompt further investigation to identify the underlying causes. Additional tests, such as a complete blood count with differential, may be conducted to gain a more comprehensive view of white blood cell populations and rule out other potential issues.
Monocytosis and monocytopenia represent opposing ends of the spectrum when it comes to monocyte counts. These conditions can be valuable indicators of an individual's health and immune function. Understanding the potential causes of these conditions is essential for healthcare professionals, as it enables accurate diagnosis and appropriate treatment planning. Regular monitoring of monocyte counts can aid in tracking progress and ensuring the best possible care for patients.
Monocytes and Autoimmune Diseases
In autoimmune diseases, the immune system loses its ability to distinguish between foreign invaders (like bacteria or viruses) and the body's own cells. This confusion leads to an immune attack on healthy tissues, causing inflammation, tissue damage, and a range of symptoms. Monocytes are directly involved in this process:
- Inflammation: Monocytes can migrate to inflamed tissues in response to signals from the immune system. In autoimmune diseases, the presence of monocytes at the sites of inflammation contributes to tissue damage and exacerbates symptoms.
- Antigen Presentation: Monocytes are proficient antigen-presenting cells. They capture antigens (pieces of foreign or self-proteins) and present them to other immune cells, such as T lymphocytes. This process can trigger or amplify autoimmune responses.
- Cytokine Production: Monocytes produce cytokines, signaling molecules that regulate the immune response. Dysregulated cytokine production by monocytes can promote inflammation and autoimmune reactions.
Monocytes in Specific Autoimmune Diseases:
Different autoimmune diseases involve varying mechanisms, but monocytes play a role in many of them:
- Rheumatoid Arthritis: Monocytes infiltrate the synovial membrane in the joints, contributing to inflammation and tissue damage.
- Systemic Lupus Erythematosus (SLE): Monocytes in SLE patients can produce excess pro-inflammatory cytokines, contributing to the systemic inflammation seen in this disease.
- Multiple Sclerosis (MS): Monocytes are involved in the breakdown of the blood-brain barrier in MS, allowing immune cells to enter the central nervous system and cause damage.
- Type 1 Diabetes: Monocytes participate in the immune attack on insulin-producing cells in the pancreas.
- Inflammatory Bowel Disease (IBD): Monocytes contribute to the intestinal inflammation seen in Crohn's disease and ulcerative colitis.
Therapeutic Implications:
Understanding the role of monocytes in autoimmune diseases offers potential therapeutic avenues:
- Targeted Therapies: Researchers are developing medications that specifically target monocytes or their products to modulate the immune response in autoimmune diseases.
- Immune-Modulating Drugs: Existing immunosuppressive drugs can impact monocyte function, and understanding these effects helps tailor treatment strategies.
- Biomarkers: Monocyte-related biomarkers can aid in diagnosing and monitoring autoimmune diseases, allowing for more precise disease management.
Monocytes in Cancer Diagnosis
Researchers have increasingly recognized that changes in monocyte levels and function can provide valuable insights into cancer diagnosis and prognosis. Here's how monocytes are being leveraged in the field of oncology:
- Tumor-Associated Macrophages (TAMs): Macrophages derived from monocytes can infiltrate tumor tissues, becoming part of what's known as the tumor microenvironment. These TAMs influence tumor growth, metastasis, and the response to therapies. Studying TAMs can provide valuable information about cancer progression.
- Inflammatory Response: Cancer often triggers an inflammatory response in the body. Monocytes are involved in this response and can release inflammatory molecules. Monitoring levels of these molecules, such as C-reactive protein (CRP), can indicate the presence and extent of cancer.
- Immune Profiling: High-throughput techniques like flow cytometry and single-cell RNA sequencing enable researchers to analyze the composition and functional state of immune cells, including monocytes, in cancer patients. This immune profiling can aid in diagnosis and predict treatment responses.
- Biomarker Discovery: Researchers are identifying specific markers on monocytes that are associated with certain cancer types. These biomarkers can be used to develop diagnostic tests and monitor treatment responses.
Applications in Cancer Types:
Monocyte-based diagnostics and research have shown promise in various cancer types:
- Breast Cancer: Studies have explored the role of monocytes and TAMs in breast cancer progression and therapy resistance.
- Lung Cancer: Monocyte-derived cells have been implicated in lung cancer metastasis and as potential therapeutic targets.
- Colorectal Cancer: Research has highlighted the importance of monocytes and macrophages in the development and progression of colorectal cancer.
- Pancreatic Cancer: Monocyte-based biomarkers are being investigated for early detection and monitoring of pancreatic cancer.
- Blood Cancers: Monocytes play a role in various blood cancers, and their analysis can aid in disease classification and monitoring.
Challenges and Future Directions:
While the potential of monocyte-based diagnostics in cancer is exciting, challenges remain. Standardizing methods for monocyte analysis, addressing heterogeneity in tumor microenvironments, and translating research findings into clinical practice are ongoing efforts.
Treatment and Management
Depending on whether a patient presents with a concerning high monocyte count (monocytosis) or a low count (monocytopenia), healthcare professionals tailor their approaches to address the underlying causes and improve the patient's overall health and well-being.
Treatment of Monocytosis
- Addressing Underlying Causes: The first step in treating monocytosis is identifying and addressing the root cause. This may involve treating infections with appropriate antibiotics, managing inflammatory conditions with anti-inflammatory medications, or providing targeted therapy for hematological disorders or cancers.
- Immune-Modulating Drugs: In cases where monocytosis is linked to autoimmune diseases, medications that modulate the immune system's response, such as corticosteroids or disease-modifying antirheumatic drugs (DMARDs), may be prescribed.
- Chemotherapy or Targeted Therapy: When monocytosis is associated with certain cancers, such as leukemia, chemotherapy or targeted therapy drugs may be necessary to manage the malignancy.
- Lifestyle Modifications: Encouraging a healthy lifestyle, including regular exercise, a balanced diet, and stress management, can help support the immune system and overall health.
- Regular Monitoring: Patients with persistent monocytosis may require regular follow-up appointments and blood tests to monitor their condition and treatment progress.
Treatment of Monocytopenia
- Addressing Underlying Causes: Like monocytosis, treating monocytopenia involves identifying and managing the underlying causes. This may include addressing bone marrow disorders, infections, or medication-related issues.
- Medication Adjustments: If monocytopenia is due to medication side effects, healthcare providers may adjust or change the medication regimen to restore monocyte levels.
- Growth Factors: In some cases, treatment with hematopoietic growth factors, such as granulocyte-macrophage colony-stimulating factor (GM-CSF), may be considered to stimulate monocyte production.
- Transfusions: In severe cases of monocytopenia where there is a heightened risk of infection, transfusions of white blood cells, including monocytes, may be administered.
- Bone Marrow Stimulation: For bone marrow disorders, treatments such as bone marrow transplantation may be necessary to restore normal hematopoiesis and monocyte production.
- Immune Support: Patients with monocytopenia may benefit from immune support measures, such as vaccinations and prophylactic antibiotics, to reduce the risk of infections.
- Lifestyle and Dietary Changes: Encouraging a well-balanced diet, proper hydration, and a healthy lifestyle can support overall immune function and assist in recovery.
Patient Education
A crucial aspect of managing conditions related to monocytes is patient education. Patients should understand the underlying causes, treatment options, and the importance of medication compliance and regular follow-up appointments. Healthcare providers play a key role in providing clear and comprehensive information to empower patients in managing their health.
Holistic Approach
It's important to recognize that the treatment and management of conditions related to monocytes often require a holistic approach. This means considering not only the specific condition but also the patient's overall health, lifestyle, and individual needs. Collaborative care involving various healthcare professionals, including hematologists, oncologists, immunologists, and primary care physicians, ensures comprehensive and patient-centered management.
Effective treatment and management of conditions related to monocytes involve addressing underlying causes, using targeted therapies when necessary, and providing ongoing support and education to patients. With advances in medical research and personalized medicine, healthcare professionals are better equipped than ever to tailor treatment plans that optimize patient outcomes and enhance their quality of life.
Conclusion
Recap of Monocyte Function and Significance
Monocytes are remarkable white blood cells with multifaceted roles in our immune system. They serve as vigilant sentinels, patrolling the bloodstream, and tissues, ready to respond to signs of infection or inflammation. When they encounter pathogens or damaged cells, they transform into potent macrophages, adept at phagocytosis and antigen presentation. This dual role allows them to both engulf invaders and communicate with other immune cells, orchestrating a coordinated immune response.
Monocytes also play a pivotal role in the innate and adaptive immune systems, bridging the gap between these two branches. They serve as a link between the immediate, nonspecific immune response and the more targeted, specific response mounted by lymphocytes. This bridge-building function is crucial for effective immunity.
Importance of Monitoring Monocyte Count
The monitoring of monocyte counts is of paramount importance in clinical medicine. An abnormal monocyte count, whether too high (monocytosis) or too low (monocytopenia), can be an early indicator of underlying health issues. Monocytosis often signals infections, inflammatory conditions, or hematological disorders, while monocytopenia may be associated with bone marrow disorders, certain medications, or severe infections.
Regular monitoring of monocyte counts can aid in early diagnosis and timely intervention, potentially preventing the progression of underlying conditions. It's a valuable tool for healthcare providers to assess the state of a patient's immune system and overall health.
Future Research Directions
Several promising avenues for future research emerge:
- Immunotherapies: Investigating how monocytes interact with emerging immunotherapies, such as checkpoint inhibitors and CAR-T cell therapies, can enhance our understanding of treatment responses and guide more effective cancer therapies.
- Single-Cell Analysis: Advancements in single-cell analysis technologies allow researchers to explore the heterogeneity of monocytes within a single individual. This can provide insights into how different monocyte subsets contribute to health and disease.
- Personalized Medicine: Tailoring treatment strategies based on a patient's monocyte profile and immune status holds immense potential for improving treatment outcomes, particularly in cancer and autoimmune diseases.
- Microbiome Interactions: Exploring the connections between the gut microbiome, monocyte function, and immune responses can uncover novel approaches to modulating the immune system and maintaining health.
- Nanomedicine: Investigating the use of nanotechnology to deliver therapeutic agents specifically to monocytes or macrophages in order to modulate immune responses and treat diseases.
In the coming years, as research into monocytes continues to expand, we can anticipate breakthroughs that not only deepen our understanding of these versatile immune cells but also translate into improved diagnostic and therapeutic approaches. The journey into the intricate world of monocytes is far from over, and it promises to unlock new avenues for enhancing human health and combating diseases.
Cite this page:
- Comment
- Posted by Dayyal Dg.