Hyaline Casts in Urine: Causes, Symptoms, Diagnosis, and Treatment
Hyaline casts in urine can indicate kidney health issues. Learn about causes, diagnosis, and treatment options.

Hyaline casts are cylindrical structures primarily made of Tamm-Horsfall mucoprotein (uromodulin), a glycoprotein secreted by renal tubular epithelial cells. They form within the distal convoluted tubules and collecting ducts of the nephron. Casts are the only element found in urinary sediment that is unique to the kidney. They are normally absent in urine or present in low numbers, usually from 0 to 2 per low-power field. Elevated levels may suggest disease, e.g., kidney stress, prerenal azotemia, dehydration, or early renal dysfunction.
How Do Hyaline Casts Appear in Urine?
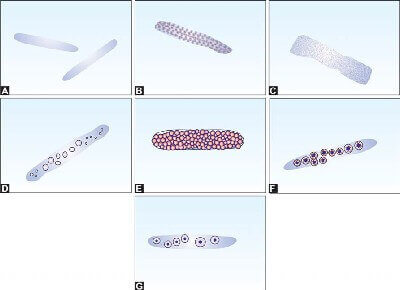
They are translucent, cylindrical structures that can only be seen through microscopic examination of the urine sediment. The renal tubules of kidneys have a cylindrical structure, which is why hyaline casts appear cylindrical in urine. They have smooth edges and a uniform texture and are often difficult to see in low-intensity light or phase-contrast microscopy. They lack cellular material, which makes them appear “glassy” or nearly invisible in bright field microscopy. Any elements in the tubular filtrate, including cells, bacteria, granules, pigments, and crystals, may become embedded within the cast matrix to form various other cast types. Urinary casts are classified into two categories: cellular casts and acellular casts. Since hyaline casts do not have any cellular components, they are categorized into acellular type of cast.
| Acellular Casts | Cellular Casts |
|---|---|
|
|
| Type of Cast | Composition | Indication |
|---|---|---|
| Hyaline | Tamm-Horsfall protein | Normal or mild kidney stress |
| Granular | Cellular debris | Acute tubular necrosis, glomerulonephritis |
| Waxy | Degenerated cells | Advanced kidney disease |
| Fatty | Lipids | Nephrotic syndrome |
| Red Cell | Red blood cells | Glomerular bleeding |
| White Cell | White blood cells | Infection or inflammation |
| Epithelial | Renal tubular cells | Tubular damage |
Clinical Significance
The presence of 0 to 2 hyaline casts per low-power field (LPF) is considered normal, as mild dehydration or physical exercise can lead to a moderate presence of hyaline casts in the urine. A level above this range may indicate kidney-related issues. Some physiological and pathological conditions are associated with an increased amount of hyaline casts in urine.
Physiological Causes
- Dehydration: It is a physiological condition in which fluid intake is low, or body loses or uses more fluid than it takes in. In such condition urine concentration increases, which may lead to hyaline cast formation.
- Intense Exercise: It increases the secretion of Tamm-Horsfall mucoprotein (uromodulin), leading to the formation of hyaline cast.
- Fever and Stress: In fever, body temperature rises, which may also cause dehydration. Physiological stress or febrile conditions can cause a temporary increase in hyaline cast formation, which indicates renal tubular response to systemic stress.
- Diuretic Use: Diuretics are medicines that increases the excretion of water and electrolytes and enhance urine flow, which may cause dehydration and increase urine concentration.
Pathological Causes
- Acute Glomerulonephritis: In this condition, inflammation of the glomeruli occurs, which often causes blood and protein in the urine and can lead to the formation of various types of casts, including hyaline casts.
- Pyelonephritis: It is a serious bacterial infection of the kidneys that causes inflammation and damage to the renal tubules. As a result, hyaline casts are formed including other cellular casts.
- Chronic Renal Disease: As the name suggests, it is a progressive and long-standing damage to kidney structures that reduces filtration and tubular function. This condition is frequently associated with persistent hyaline cast formation in the urine.
- Acute Kidney Injury: AKI refers to a sudden decline in kidney function, leading to the accumulation of waste products and decreased urine output. This can concentrate the urine and increase the formation of hyaline casts.
- Prerenal Azotemia: This condition is often caused by dehydration or reduced cardiac output. As a result, blood flow to the kidneys decreases. The reduced perfusion leads to concentrated urine, which may contain hyaline casts.
- Congestive Heart Failure: In CHF, the heart reduces its pumping efficiency and limits blood flow to the kidneys, which can cause fluid retention and concentrated urine. Both of these conditions favor the development of hyaline casts.
- Diabetic Nephropathy: In this condition, the kidneys are damaged as a complication of long-term diabetes. It is commonly marked by proteinuria and tubular stress, often accompanied by hyaline casts.
- Meningitis: It is a serious medical condition characterized by inflammation of the protective membranes (meninges) surrounding the brain and spinal cord caused by bacterial or viral infections. Although it primarily affects the central nervous system, severe systemic infections like meningitis can trigger a widespread inflammatory response. This condition can cause physiological stress on the kidneys, potentially leading to reduced renal perfusion and tubular injury. As a result, hyaline casts may appear in the urine due to increased Tamm-Horsfall protein secretion and concentration in the renal tubules.
Symptoms
If you have hyaline casts in your urine, there are no symptoms. However, there may be some underlying conditions, such as swelling (edema), reduced urine output, or blood in your urine (hematuria).
Diagnosis
For the diagnosis of hyaline casts in urine, a microscopic examination of the urine sediment is carried out. A spot urine sample is collected in a clean, sterile container, and the lab technician observes the urine sample under a microscope for the presence of hyaline casts. This test is a part of routine urinalysis. Your doctor may order this test if any kidney issues are suspected.
Treatment
- Ensure adequate hydration: Increasing fluid intake is helpful for the correction of dehydration, which is the common cause of hyaline cast formation.
- Manage underlying conditions: A proper medical treatment is necessary for acute kidney injury (AKI), chronic kidney disease (CKD), or systemic stress to reduce cast formation.
- Review medications: Diuretics often causes the increases of urine concentration that may be concentrating your urine too much, your doctor might need to adjust your prescription.
- Give your body time to recover: When hyaline casts appear due to things like intense exercise, fever, or physical stress, simply resting and taking care of yourself is often enough.
- Follow up with testing: Your doctor may recommend follow-up tests, including urinalysis and kidney function tests such as urea, blood urea nitrogen (BUN), creatinine, and electrolytes, to monitor your kidney health.
Takeaways
- Hyaline casts in urine are common and can indicate kidney health status.
- Normal levels are 0–2 per LPF; higher levels may require medical attention.
- Causes include dehydration, exercise, and kidney diseases like AKI or CKD.
- Diagnosis is performed through microscopic urinalysis, a common laboratory test of urine.
- Treatment involves hydration, diet, and monitoring underlying conditions.
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Reference(s)
- Shikata, Elisa., et al. “The Detection of Hyaline Casts in Patients Without Renal Dysfunction Suggests Increased Plasma BNP.” EJIFCC, vol. 32, no. 4, pp. 410-420., pmid: 35046759. <https://pmc.ncbi.nlm.nih.gov/articles/PMC8751402/>.
- Cavanaugh, Corey., et al. “Urine Sediment Examination in the Diagnosis and Management of Kidney Disease: Core Curriculum 2019.” American Journal of Kidney Diseases, vol. 73, no. 2, 21 September 2018, pp. 258-272., doi: 10.1053/j.ajkd.2018.07.012. <https://doi.org/10.1053/j.ajkd.2018.07.012>.
- Hernández, Anna. “Hyaline Casts: What Are They, Causes, Diagnosis, Treatment, and More.” Osmosis from Elsevier <https://www.osmosis.org/answers/hyaline-casts>.
- Ringsrud, K. M.. “Casts in the Urine Sediment.” Laboratory Medicine, vol. 32, no. 4, 01 April 2001, pp. 191-193., doi: 10.1309/kj5e-v5fe-mahr-kxt2. <https://doi.org/10.1309/kj5e-v5fe-mahr-kxt2>.
Cite this page:
- Posted by Dayyal Dungrela