Examination of Blood Smear
Discover how blood smears are analyzed for red blood cells, white blood cells, platelets, and parasites. Learn the role of different magnifications in diagnosing anemia, infections, and blood disorders.

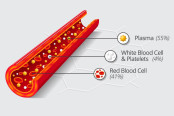
A blood smear is systematically analyzed to assess several key cellular components:
- Red Blood Cells (RBCs): The examination focuses on morphology, identifying immature forms, inclusion bodies, and the overall arrangement of cells. This helps in detecting conditions like anemia and other hematological disorders.
- White Blood Cells (WBCs): A differential count is conducted to categorize the various types of white cells, paying particular attention to any abnormal or immature forms, which may indicate infections, leukemias, or immune responses.
- Platelets: The adequacy of platelets, as well as the presence of any abnormal forms, is evaluated. This assessment is crucial for diagnosing disorders that affect blood clotting.
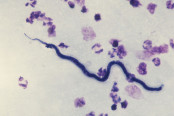
- Parasites: Specific attention is given to detecting blood-borne parasites, such as those responsible for malaria and filariasis. The identification of these parasites is essential for diagnosing and managing these infections.
A peripheral blood smear typically comprises three distinct regions: the head, body, and tail. For optimal analysis, the smear should be observed under different magnifications. Initially, a low power objective (10×) is used to evaluate the overall quality of the smear, including the distribution and staining of cells. This also allows for the identification of cell clumping (e.g., Rouleaux formation) and the detection of microfilariae.
For detailed analysis, particularly of red blood cell morphology and to perform a differential leukocyte count, the high power objective (45×) is preferred. This magnification also provides a preliminary estimate of the total white blood cell count, which can be cross-referenced with manual or automated counts.

Finally, the oil-immersion objective (100×) is utilized for an in-depth examination of any abnormal cells. This step is critical for identifying subtle morphological changes that could indicate specific hematological conditions.
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Cite this page:
- Posted by Dayyal Dungrela
From Around The Web
-

Life Cycle of Malaria Parasite
Microbiology -
Microscopic Examination of Blood for Demonstration of Microfilaria
Microbiology -
Morphology of Platelets
Hematology -
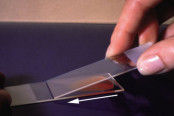
PREPARATION OF BLOOD SMEAR (WEDGE METHOD)
Microbiology -

Red Blood Cells Morphology
Hematology -

White Blood Cells Morphology
Hematology