Red Blood Cells Morphology
Learn about RBC morphology, including abnormal RBC size, shape, and staining patterns, to better understand various anemias like microcytic, macrocytic, and hemolytic.

To accurately assess red blood cells (RBCs) morphology, the best examination occurs in areas where the cells are slightly touching one another, typically towards the tail end of the blood film. Normal RBCs are approximately 7-8 μm in diameter, exhibit a smooth, round shape, and display a deep pink stain at the periphery with a paler center. The central pallor typically occupies about one-third of the cell's diameter. These normocytic (normal size) and normochromic (normal hemoglobin content) RBCs closely match the size of the nucleus of a small lymphocyte.
Box 1: Role of blood smear in anemias
- Macrocytic Anemia: Differentiation is necessary between conditions such as megaloblastic anemia (characterized by oval macrocytes and hypersegmented neutrophils), liver disease (round macrocytes and target cells), hemolytic anemia (presence of numerous polychromatic cells), and myelodysplastic syndrome (featuring dimorphic RBCs, pseudo-Pelger-Huet neutrophils, giant platelets, and occasional blast cells).
- Microcytic Anemia: This involves distinguishing between iron deficiency anemia (microcytic hypochromic RBCs, pencil cells), thalassemia minor (microcytic hypochromic RBCs with basophilic stippling), and sideroblastic anemia (dimorphic anemia).
- Sickle Cell Disease: Differentiation is made between sickle cell trait (target cells without sickle cells), sickle cell anemia (presence of sickle cells), and sickle cell B-thalassemia (microcytic hypochromic RBCs and sickle cells).
- Hemolytic Anemias: Characterized by the presence of spherocytes (seen in hereditary spherocytosis and autoimmune hemolytic anemia), fragmented cells (indicative of microangiopathic hemolytic anemia), and bite or blister cells (common in glucose-6-phosphate dehydrogenase deficiency).
Abnormal Red Blood Cell Morphology
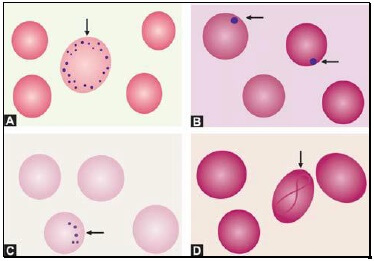
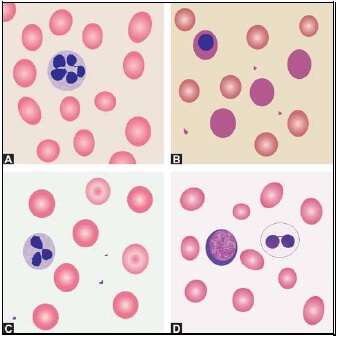
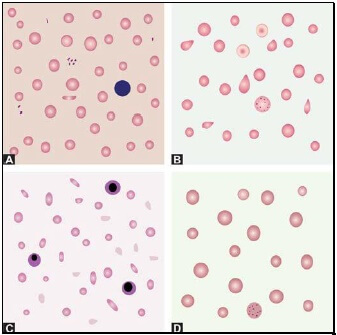
Abnormalities in RBC morphology can be categorized based on size (see Figure 1), staining properties, shape (see Figure 1), inclusions (see Figure 2), and arrangement (see Figure 4).
Abnormal RBC Size
While minor variations in RBC size are common, significant changes indicate anisocytosis, a hallmark of many anemias. Anisocytosis results from the presence of microcytes, macrocytes, or both.
- Microcytes: These are smaller-than-normal RBCs and are commonly seen when hemoglobin synthesis is impaired, as in iron deficiency anemia, thalassemias, and sideroblastic anemia.
- Macrocytes: Larger-than-normal RBCs, often seen in megaloblastic anemia, myelodysplastic syndrome, and patients undergoing cancer chemotherapy. Oval macrocytes (macro-ovalocytes) are typical in megaloblastic anemia, whereas round macrocytes are seen in liver disease, alcoholism, and hypothyroidism.
Abnormal RBC Staining (Hemoglobin Content)
The staining intensity of RBCs is directly related to their hemoglobin content. Cells with an increased area of central pallor, indicating reduced hemoglobin, are termed hypochromic. Such cells are typically found in conditions where hemoglobin synthesis is defective, such as iron deficiency, thalassemias, and sideroblastic anemia.
Dimorphic Anemia
This condition is characterized by the presence of two distinct populations of RBCs in a single smear. Examples include the coexistence of normochromic and hypochromic RBCs in sideroblastic anemia, iron deficiency anemia responding to treatment, or following a blood transfusion in a patient with hypochromic anemia.
Abnormal RBC Shape
Variation in RBC shape, known as poikilocytosis, is indicative of various anemias.
- Sickle Cells: These elongated cells, with pointed ends, assume a sickle shape when RBCs containing hemoglobin S are deprived of oxygen. They are a key feature of sickle cell disorders, particularly sickle cell anemia.
- Spherocytes: Slightly smaller, round RBCs that stain intensely and lack the central area of pallor, indicative of hereditary spherocytosis and autoimmune hemolytic anemia.
- Schistocytes: Fragmented RBCs that take on various forms, such as helmets or crescents, often with surface projections. They are seen in microangiopathic hemolytic anemia, cardiac valve prosthesis, and severe burns.
- Target Cells: Characterized by a bull's-eye appearance with a central stained area, peripheral stained rim, and unstained cytoplasm in between, target cells are common in hemoglobinopathies like thalassemias, obstructive jaundice, and post-splenectomy.
- Burr Cells (Echinocytes): Small RBCs with regularly spaced projections on their surface, commonly seen in uremia.
- Acanthocytes: RBCs with irregularly spaced, sharp projections, often found in spur cell anemia of liver disease, McLeod phenotype, and post-splenectomy.
- Teardrop Cells (Dacryocytes): These tapering, droplike RBCs are prevalent in myelofibrosis and myelophthisic anemia.
- Blister Cells (Hemi-Ghost Cells): Cells with hemoglobin contracted away from the cell membrane, seen in glucose-6-phosphate dehydrogenase deficiency during acute hemolytic episodes.
- Bite Cells: Formed when Heinz bodies are removed by the spleen's pitting action, these cells are characteristic of glucose-6-phosphate dehydrogenase deficiency and unstable hemoglobin disease.
Red Cell Inclusions
Inclusions visible on Romanowsky-stained smears include basophilic stippling, Howell-Jolly bodies, Pappenheimer bodies, and Cabot’s rings.
- Basophilic Stippling: Indicative of impaired erythropoiesis, basophilic stippling features numerous, irregular, basophilic granules uniformly distributed in RBCs. It is seen in conditions like thalassemias, megaloblastic anemia, heavy metal poisoning, and liver disease.
- Howell-Jolly Bodies: Small, round, purple-staining nuclear remnants seen in megaloblastic anemia, thalassemias, hemolytic anemia, and post-splenectomy.
- Pappenheimer Bodies: Basophilic, iron-containing granules within RBCs that are fewer in number and not uniformly distributed, commonly seen following splenectomy and in sideroblastic anemia.
- Cabot’s Rings: Fine, reddish-purple ring-like structures indicating impaired erythropoiesis, typically seen in megaloblastic anemia and lead poisoning.

Immature Red Cells
- Polychromatic Cells: These slightly larger RBCs contain remnants of ribonucleic acid and exhibit a bluish-grey tint. Their presence is indicative of active erythropoiesis, commonly seen in hemolytic anemia, acute blood loss, and after specific therapy for nutritional anemia.
- Nucleated Red Cells: Prematurely released from the bone marrow, these erythroblasts are normal in the cord blood of newborns. However, large numbers in a blood smear suggest hemolytic disease of the newborn, hemolytic anemia, leukemia, myelophthisic anemia, or myelofibrosis.

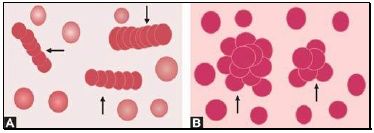
Abnormal Red Cell Arrangement
- Rouleaux Formation: This refers to the stacking of RBCs, resembling a stack of coins. It is often observed in multiple myeloma, Waldenström's macroglobulinemia, hypergammaglobulinemia, and hyperfibrinogenemia.
- Autoagglutination: The clumping of RBCs into large, irregular groups, typically seen in cold agglutinin disease.

The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Cite this page:
- Posted by Dayyal Dungrela