Common Applications of Flow Cytometry in Hematology
Explore the common applications of flow cytometry in hematology, including immunophenotyping, diagnosing leukemias and lymphomas, monitoring HIV infection, and more.
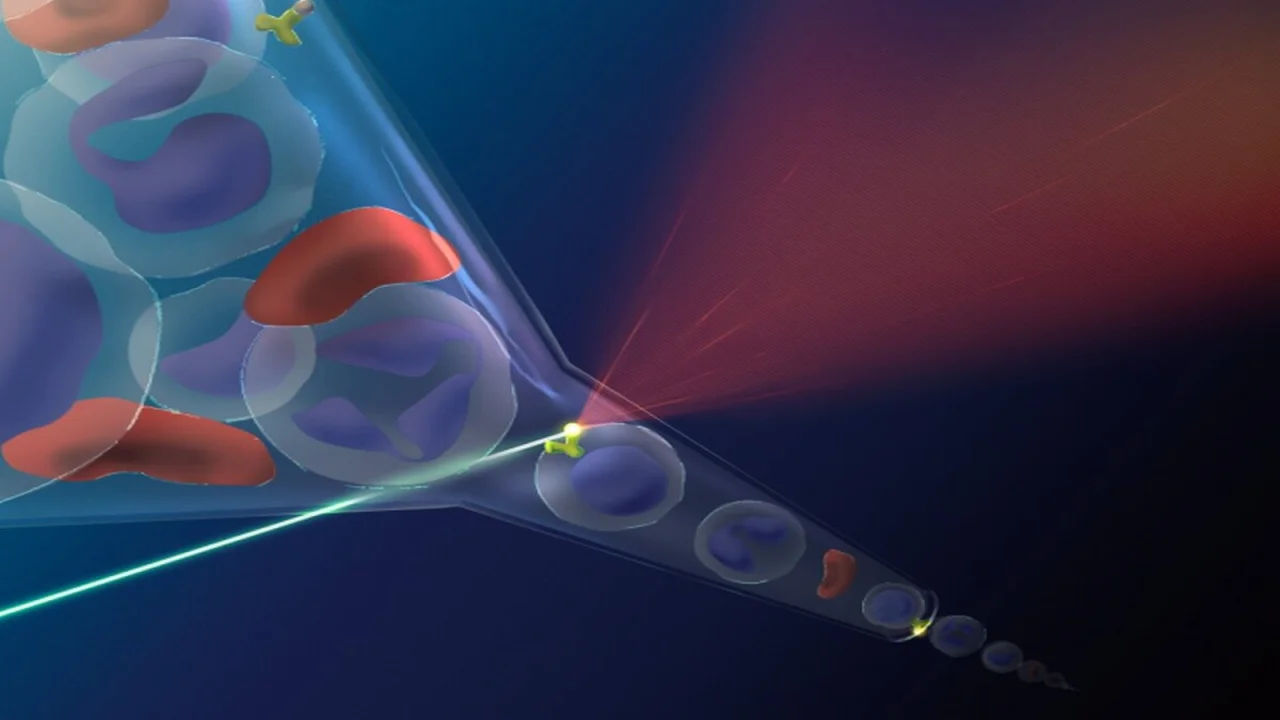
Flow cytometry is a sophisticated and essential technology widely utilized in the field of hematology. This powerful tool allows for the analysis of physical and chemical characteristics of cells in a fluid as they pass through a laser beam, making it invaluable for diagnosing and monitoring a variety of hematological disorders. The versatility of flow cytometry in hematology is evident in its numerous applications, ranging from immunophenotyping to reticulocyte counting, as well as its use in managing conditions like leukemias, lymphomas, and anemias. As medical science continues to advance, the role of flow cytometry in hematology becomes even more critical, especially in the context of modern treatments like hematopoietic stem cell transplantation and in assessing conditions such as paroxysmal nocturnal hemoglobinuria.
Immunophenotyping in Hematology
Immunophenotyping
One of the most prominent applications of flow cytometry in hematology is immunophenotyping, which involves the evaluation of cell surface markers to identify and characterize different cell populations. Immunophenotyping is crucial for diagnosing hematological malignancies, particularly leukemias and lymphomas. In these conditions, flow cytometry is used to identify specific markers on the surface of leukocytes, allowing for the classification of the malignancy and the determination of the lineage and maturation stage of the abnormal cells.
Diagnosing Leukemias and Lymphomas
In the context of leukemias and lymphomas, flow cytometry aids in the diagnosis by identifying abnormal populations of lymphoid or myeloid cells. For example, in chronic lymphocytic leukemia (CLL), flow cytometry is used to detect the co-expression of CD5 and CD19, markers that are indicative of the disease. Additionally, flow cytometry can detect minimal residual disease (MRD) after treatment, which is critical for monitoring the effectiveness of therapy and predicting relapse. By quantifying the remaining cancerous cells that are below the detection limit of traditional methods, flow cytometry provides valuable prognostic information.
Prognostic Subgroup Identification
Beyond diagnosis, immunophenotyping via flow cytometry is essential for identifying prognostically significant subgroups within hematological malignancies. For instance, certain subtypes of acute lymphoblastic leukemia (ALL) can be classified based on the expression of specific markers, which in turn can influence treatment decisions and predict outcomes. The ability of flow cytometry to rapidly and accurately analyze multiple markers simultaneously makes it a powerful tool for guiding personalized medicine in hematology.
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Detecting CD55 and CD59 Deficiency
Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired hematological disorder characterized by hemolysis, bone marrow failure, and thrombosis. Flow cytometry is the gold standard for diagnosing PNH, as it allows for the detection of deficient expression of CD55 and CD59 on red blood cells and other hematopoietic cells. The absence or reduction of these surface proteins leads to the increased susceptibility of red blood cells to complement-mediated lysis, which is the hallmark of PNH.
Clinical Relevance
The ability to accurately diagnose PNH through flow cytometry has profound clinical implications. Patients with PNH often present with nonspecific symptoms, and a delay in diagnosis can lead to severe complications. Flow cytometry not only confirms the diagnosis but also quantifies the proportion of affected cells, which is important for assessing disease severity and guiding treatment decisions. Regular monitoring of PNH clones via flow cytometry is also crucial for evaluating the effectiveness of therapies, such as eculizumab, that target the complement pathway.
Hematopoietic Stem Cell Transplantation
Enumeration of CD34+ Stem Cells
Hematopoietic stem cell transplantation (HSCT) is a life-saving procedure for patients with certain hematological malignancies, bone marrow failures, and genetic disorders. The success of HSCT largely depends on the number and viability of transplanted stem cells, which are typically identified by the expression of the CD34 marker. Flow cytometry is the preferred method for enumerating CD34+ stem cells in peripheral blood or bone marrow before transplantation.
Ensuring Successful Transplantation
Accurate quantification of CD34+ cells is critical for determining the appropriate timing for stem cell collection and the likelihood of engraftment success. Flow cytometry offers a rapid, reliable, and reproducible means of assessing stem cell counts, ensuring that sufficient cells are harvested for transplantation. Moreover, flow cytometry can be used to monitor the reconstitution of the hematopoietic system post-transplantation, providing early indications of graft success or failure.
Feto-Maternal Hemorrhage
Detection of Fetal Hemoglobin in Maternal Blood
Feto-maternal hemorrhage (FMH) occurs when fetal blood cells enter the maternal circulation, which can lead to complications such as alloimmunization and hemolytic disease of the fetus and newborn (HDFN). Flow cytometry is highly effective in detecting and quantifying fetal hemoglobin (HbF) in a maternal blood sample, which is crucial for diagnosing and managing FMH.
Clinical Importance
In cases of suspected FMH, flow cytometry provides a sensitive and specific method for detecting even small volumes of fetal blood in the maternal circulation. This information is vital for determining the appropriate dose of anti-D immunoglobulin in Rh-negative mothers to prevent sensitization. Additionally, in cases where FMH is detected late in pregnancy, flow cytometry can guide the decision-making process regarding the need for intrauterine transfusions or early delivery to manage fetal anemia.
Anemias and Reticulocyte Count
Role of Flow Cytometry in Anemia Diagnosis
Flow cytometry is a valuable tool in the evaluation of various anemias, particularly through the measurement of the reticulocyte count. Reticulocytes are immature red blood cells that are released from the bone marrow into the bloodstream, and their count serves as an indicator of erythropoietic activity. Flow cytometry provides a precise and automated method for counting reticulocytes, which is important for distinguishing between different types of anemia.
Diagnostic Applications
In hemolytic anemias, where there is increased destruction of red blood cells, the reticulocyte count is typically elevated as the bone marrow compensates by producing more red blood cells. Conversely, in conditions like aplastic anemia or iron deficiency anemia, the reticulocyte count may be low, indicating reduced erythropoiesis. Flow cytometry allows for the rapid and accurate quantification of reticulocytes, aiding in the differential diagnosis of anemia and guiding appropriate treatment strategies.
Human Immunodeficiency Virus (HIV) Infection
Enumeration of CD4+ Lymphocytes
In the management of human immunodeficiency virus (HIV) infection, flow cytometry is widely used to enumerate CD4+ lymphocytes, a key marker of immune function. The CD4+ T-cell count is a critical parameter for assessing the stage of HIV infection, determining the initiation of antiretroviral therapy (ART), and monitoring the immune response to treatment.
Importance in Clinical Management
The depletion of CD4+ cells is a hallmark of HIV infection, and regular monitoring of CD4+ counts via flow cytometry is essential for predicting disease progression and the risk of opportunistic infections. Flow cytometry provides a precise and reproducible method for measuring CD4+ lymphocyte levels, enabling clinicians to tailor treatment regimens to individual patients and optimize their care. Moreover, CD4+ counts are used to determine eligibility for certain prophylactic therapies and to assess the effectiveness of ART in restoring immune function.
Histocompatibility Cross-Matching
Role in Transplantation
Histocompatibility cross-matching is a crucial step in the organ transplantation process, where flow cytometry is used to detect the presence of donor-specific antibodies in the recipient’s blood. These antibodies, if present, can lead to graft rejection. Flow cytometry-based cross-matching offers higher sensitivity and specificity compared to traditional methods, making it the preferred technique for pre-transplant evaluation.
Enhancing Transplant Outcomes
By providing detailed information on the compatibility between donor and recipient, flow cytometry helps reduce the risk of acute and chronic rejection, ultimately improving transplant outcomes. The ability to identify low levels of donor-specific antibodies that might be missed by other methods allows for better selection of compatible donors and the implementation of strategies to manage sensitized recipients, such as desensitization protocols or the use of immunosuppressive therapies.

The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Cite this page:
- Posted by Dayyal Dungrela