Blood Clot in Brain: Reason, Causes, Symptoms & Treatment
Explore the precise symptoms of blood clotting in the brain. Learn how to identify and understand these critical neurological signs.
Living in an era of rapidly evolving medical knowledge, it's crucial for the general public to understand common medical conditions and how they could be affected. One such condition, forming blood clots in the brain, can have significant health implications if not promptly identified and managed. This concept is explored through various facets including the physiological mechanisms responsible for clot formation, potential adverse outcomes if left untreated, recognizable symptoms and early warning signs, contemporary diagnostic and therapeutic methods, and practical preventative strategies for reducing risk.
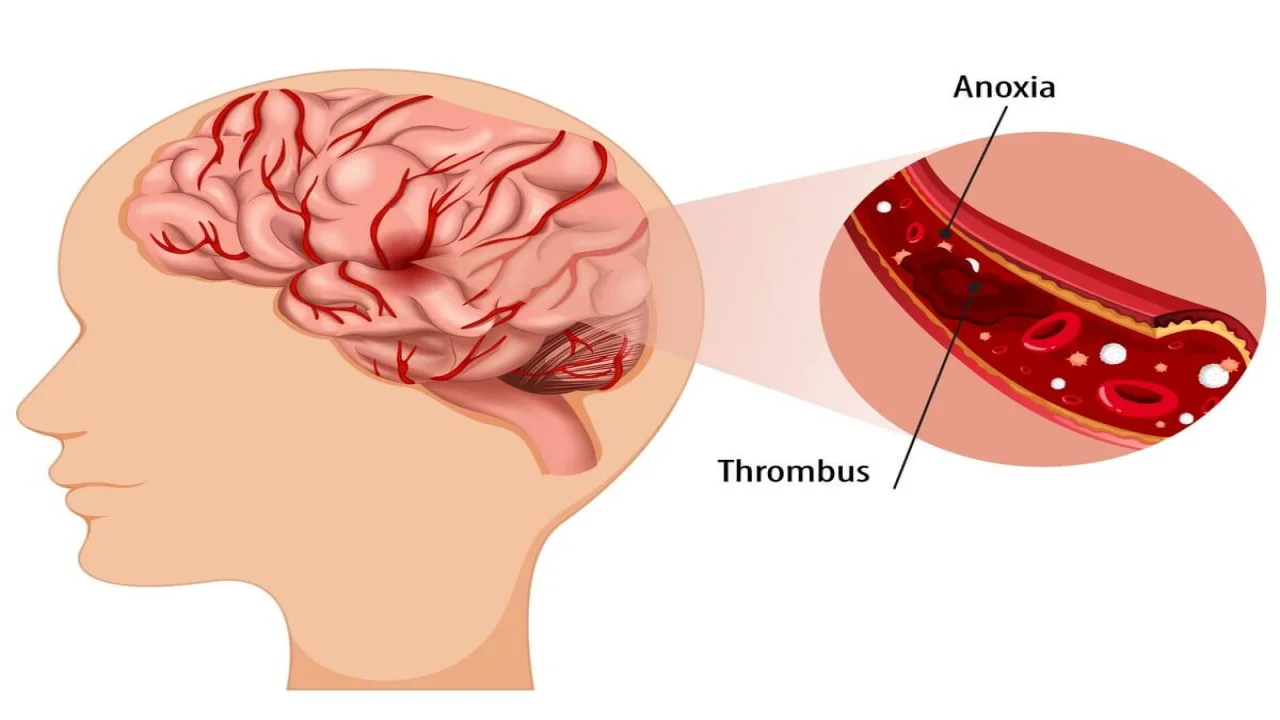
The Mechanisms of Blood Clot Formation
The process of blood clot formation in the brain, commonly referred to as thrombosis, is complex, nuanced, and deeply influenced by a multitude of factors. The being said, it is indispensable to have an understanding of these influences to facilitate future research aimed at developing and refining treatment strategies for cerebrovascular disorders.
Blood clot formation takes place through a sequence of events, most notably platelet aggregation and activation of the coagulation cascade, both of which have the potential to lead to thrombosis. However, these processes do not occur in isolation; they are regulated and affected by numerous factors, including the genetic make-up of an individual, environmental influences, and health conditions.
Genetic factors can manifest as inherited thrombophilias, such as Factor V Leiden mutation or the prothrombin gene mutation, which enhance the propensity for clot formation. Mutations in these genes increase the risk due to their role in regulating the balance between thrombosis and hemostasis. Similarly, the ABO blood type system plays a critical role. Recent research has unveiled interesting results: those with non-O blood groups might bear an elevated risk for certain thromboembolic disorders, including stroke. It appears that the blood type can influence the levels of certain clotting factors in the bloodstream, thereby modulating the propensity for thrombosis.
Environmental factors, especially lifestyle choices, play an equally important and interlinked role in clot formation. Smoking and alcohol abuse, for instance, are associated with higher rates of thrombosis, while lack of physical activity and a diet that is high in saturated fats can influence blood platelet activity and subsequently trigger clot formation.
Existing health conditions such as diabetes, hypertension, and high cholesterol can escalate the risk of blood clot formation, while diseases that compromise the vascular endothelium like atherosclerosis, drastically increase the chance of clot occurrence. Furthermore, certain medications or treatments such as hormone replacement therapy or contraceptive pills also contribute to the thrombosis risk spectrum by increasing blood viscosity or altering coagulation proteins.
The complexity of blood clot formation in the brain is further compounded by age and gender. Generally, aging escalates the risk due to physiological changes like reduced vessel elasticity and slower blood flow. Gender also inflects risk, with women during reproductive years facing a higher likelihood due to estrogen levels, a hormone found to promote clot formation.
Evidently, blood clot formation in the brain can be triggered and influenced by myriad deeply interlinked factors — an intricate ballet of genetic, environmental, medical and physiological cues. Grasping this multilayered process in its totality is a challenging endeavor, but an essential one as we strive to advance our understanding, diagnosis, and treatment strategies for thrombotic disorders.
Adverse Consequences: Stroke and Beyond
Blood clots in the brain, or cerebral clots, not only induce stroke but can also manifest in numerous ways, leading to a gamut of complications. A firm grasp of these clinical presentations and complications is quintessential in elucidating the fundamental pathologies in stroke. This element of understanding assists in both prediction and immediate treatment processes.
Delving into the direct correlation between cerebral clots and strokes, the headway point is the critical role the clot plays. It obstructs the blood flow, causing an ischemic stroke, the most common type of stroke. A lack of blood flow results in inadequate oxygen supply to parts of the brain served by the blocked artery, subsequently causing neuronal death or cerebral infarction. This triggering of neuronal death significantly impacts brain function, as areas of the brain are specialized for particular tasks.
Following the stroke, immediate and post immediate complications often arise, varying from physical, cognitive to emotional changes. Physiologically, neurologic deficits tend to manifest, such as the loss of mobility or inability to control one side of the body, commonly referred to as hemiparesis. High incidences of seizures and language impairment known as aphasia have been recorded, and while rarer, visual disturbances or visual field losses can also occur.
In this complex matrix, cognitive impairments often intertwine with physical changes. Post-stroke individuals may exhibit a decrease in alertness or changes in judgment and attention span. Disruptions in memory, spatial cognition, and executive functions such as planning and reasoning can be common, severely impacting the survivor’s daily activities and quality of life.
Notably, emotional tolls are closely linked to these physical and cognitive changes. Known as Post Stroke Depression (PSD), this common emotional disorder amongst stroke survivors is closely linked to worsening recovery progress, increased disability, and potentially higher mortality rates.
As a consequence of stroke, additional complications such as pneumonias, deep vein thrombosis - 'clots in the legs', and cardiac issues can arise as the body adjusts to the damage inflicted. Bedridden patients, particularly, might face the risk of bedsores or pressure ulcers.
Significant research continues to tackle this debilitating health challenge at its roots - understanding and preventing clot formation. Nonetheless, recognizing the wideranging complications induced by cerebral blood clots remains a cornerstone in managing these thrombotic disorders. It forms a significant portion of comprehensive patient care – from anticipation and prevention of secondary complications to rehabilitating and supporting individuals for recovery and improved quality of life. In this advancements in knowledge instigates hope, even in face of such multifaceted complications.
Symptoms and Early Warning Signs
The inherent complexity of detecting a cerebral clot lies in its primarily covert nature. Given that about 50% of these clots in the brain, medically known as cerebral venous sinus thrombosis (CVST), do not exhibit any symptoms until a significant proportion of the brain is affected, swift and accurate determination can often mean the difference between life and death. Multiple neurological symptoms can indicate a potential cerebral clot, warranting both clinical suspicion and agile responses.
Severe headaches stand as quintessential indicators. This portentous symptom is usually described as the 'worst headache of one's life,' and unlike typical migraines or tension headaches, do not succumb to over-the-counter analgesics. This type of headache is often associated with other neurological symptoms.
Neurological signs vary based on the location and extent of the clot. Hemiparesis or weakness of one side of the body, as well as seizures, are noticeable indicators. Nevertheless, sudden onset of these signs in an individual with no prior history may heighten suspicions of a potential clot.
Visual disturbances, such as partial vision loss or double vision, similarly underscore the seriousness of these signs. Sensitivity to light or blurred vision may also occur, and any significant abrupt changes in vision ought not to be dismissed.
Aphasia, a marked impairment of language ability, further serves as a red flag. An abrupt onset of difficulty in speaking, understanding speech, or inability to read or write, suggests immediate medical examination.
Cognitive impairments, both subtle and profound, may hint at a cerebral clot. The involved cognitive domains may include memory, spatial cognition, and executive functions, such as organizing, planning, and problem-solving.
Significant behavioral changes, including lethargy, unsteady gait, loss of consciousness, or falling into a coma, play an integral role in diagnosis. The person might experience abrupt and significant alterations in consciousness, including confusion or even loss of consciousness, warranting immediate medical attention.
Additionally, neurological symptoms could couple with systemic symptoms of thrombosis, such as fever. This combination may arise due to the inflammatory response to the presence of the clot.
While these symptoms may indicate the presence of a potential cerebral clot, it is fundamental to note that their absence does not preclude the existence of such a clot. Given the complex nature of the brain's response to ischemia and the varied responses of different brain areas to blood flow disruption, it is critical to approach each case with clinical suspicion and a comprehensive approach.
Moreover, prevention and early detection strategies tailored to the individual's risk factors, derived from their genetic predisposition, lifestyle choices, and overall health history, are paramount to tackling cerebral thrombosis effectively. Collaborative efforts to enhance understanding, diagnosis, and treatment of cerebral thrombosis promise improved patient outcomes and the prospect of a future where no one is blindsided by this insidious condition. The pursuit of knowledge and scientific exploration in the realm of cerebral clots propels us forward, ever itching closer to the goal of prevention, precise diagnosis, and effective therapy.
Diagnostic and Therapeutic Approaches
Today’s rapidly advancing technologies and evolving medical methodologies allow an increasingly precise diagnosis of cerebral thrombosis. Modern techniques now enable efficient detection of even the subtlest blood clots within the brain's intricate vascular network.
Imaging technology, in particular, plays a pivotal role in an era where a high degree of precision and accuracy is paramount. Techniques such as Computerized Tomography (CT) scans and Magnetic Resonance Imaging (MRI) have become indispensable in the medical fraternity. Indeed, these high-resolution techniques provide detailed, cross-sectional views of the brain structure. The affliction site, clot size and spatial relationship with surrounding structures can be effectively elucidated, removing much of the uncertainty surrounding cerebral thrombotic diagnosis.
Similarly significant is the advent of CT venography and MR venography, now considered gold standards for diagnosing cerebral venous sinus thrombosis. These imaging techniques allow visualization of the brain's venous system, drastically enhancing diagnostic precision.
Further complementing these mainstream imaging techniques have been digital subtraction angiography and transcranial Doppler ultrasound. The former technique provides a visualization of the blood vessels in the brain by subtracting the bone and soft tissue images, while the latter quantifies the velocity and direction of blood flow in the intracerebral arteries.
On the therapeutic front, anticoagulant medication has emerged as the most common treatment for cerebral thrombosis. Medications such as heparin and warfarin have proven exceptionally influential in thwarting clot growth and preventing further coagulation.
Intravenous tissue plasminogen activator (tPA), a potent clot-busting drug, is often prescribed in ischemic stroke for patients who reach healthcare facilities within a stipulated "golden hour." The application of this thrombolytic therapy shows significant success in restoring the blood flow drastically increasing chances of a full recovery.
In rare but severe cases where the clot endangers life due to its sheer size or location, surgery may be an imminent option. Endovascular mechanical thrombectomy deploys tiny devices through the network of blood vessels and physically removes the clot, restoring the blood flow.
Undeniably, the advent of these advanced technologies and methodologies has reshaped the diagnosis and management of cerebral thrombosis. However, the key lies in a prompt and accurate diagnosis coupled with personalized treatment strategies, and in there lies the need for continuous research, innovation, and improvement in this field. Indeed, such an investment in the better understanding and management of cerebral thrombosis will undoubtedly contribute to dwindling global stroke statistics and advance the overall health of society.
Preventative Strategies and Lifestyle Changes
With the intricacies and complexities of cerebral thrombosis thoroughly elucidated, we delve now into the ways which lifestyle modifications and preventative measures can mitigate the risk of experiencing this life-threatening condition. The instrumentality of these improvements extends beyond averting cerebral thrombosis but into ameliorating overall health and quality of life, thereby reinforcing the importance of these practices.
Arguably, dietary modification ranks significantly among the major lifestyle changes that can effectively reduce the risk of blood clotting in the brain. Notably, a diet rich in fruits, vegetables, whole grains, and lean proteins, particularly the Mediterranean diet, has been extensively linked to a lower incidence of cardiovascular diseases that readily precipitate cerebral thrombosis. The scientific community attributes this lower risk to the potent anti-inflammatory and anti-thrombotic properties of the nutrients inherent in this diet.
Simultaneously, it is essential to reduce the intake of sodium, trans fats, and saturated fats, known to elevate blood pressure and cholesterol levels. These, in turn, can accelerate platelet aggregation processes and enhance the risk of clotting. Likewise, excessive alcohol consumption directly impacts coagulation factors and platelet activation, potentiating cerebrovascular thrombotic disorders.
On a parallel stream runs the importance of maintaining a healthy weight. Obesity, a global health menace, heightens the risk of developing clots by causing a state of chronic inflammation and hypercoagulability. Effective weight management strategies, including regular exercise and a balanced diet, can mitigate these risk factors significantly.
Physical exercise, a non-negotiable facet of a healthy lifestyle, plays a crucial role in primary and secondary prevention of cerebrovascular diseases. Regular moderate-to-vigorous exercise improves cardiovascular health, allows for proper blood circulation, and aids in weight management. Additionally, physical activity exhibits a protective effect by reducing inflammation, endothelial dysfunction, and oxidative stress—all significant precursors to thrombosis.
Nicotine, a major constituent of tobacco, leads to the malfunction of the vascular endothelium precipitating an abnormal clotting scenario. Consequently, avoiding smoking and other forms of tobacco usage forms a key strategy in minimizing the risk of cerebral thrombosis.
Rightly, stress and lack of adequate sleep have been identified as silent but potent risk factors for thrombotic disorders. Continuous research underscores the connection between enduring stress, disturbed sleep patterns, and heightened risk of clotting disorders. Thus, stress management and good sleep hygiene form an integral part of comprehensive preventive strategies against cerebral thrombosis.
Reiteratively, it is vital to adhere to medication regimens for pre-existing conditions, such as hypertension, diabetes mellitus, and hypercholesterolemia, which indirectly increase the chances of developing cerebral clots.
The alliance between innovations in biomedical research, the integration of personalized medicine, preventive strategies, and dietary and lifestyle modifications positions us advantageously in the battle against cerebral thrombosis. The conscientious adoption of these practices promises to raise the health standards of the populace, reduce incidences of cerebral thrombosis, and improve overall health outcomes.
Armed with this information, individuals can better identify potential brain clot symptoms and seek immediate medical intervention. We've also explored the multitude of potent diagnostic tools and treatments available for managing this condition efficiently. Moreover, practical strategies for preventing the formation of these potentially life-threatening clots have been outlined, emphasizing the powerful role of lifestyle changes and pharmacological interventions. Ultimately, awareness and knowledge are the first steps towards protection and good health. The more informed we are, the better equipped we are to navigate the complex landscape of health-related issues and maintain optimal wellness.
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Cite this page:
- Posted by Dayyal Dungrela