How do you die from multiple myeloma?
Improved survival among patients with multiple myeloma is one of the most impressive cancer treatment success stories in recent years.
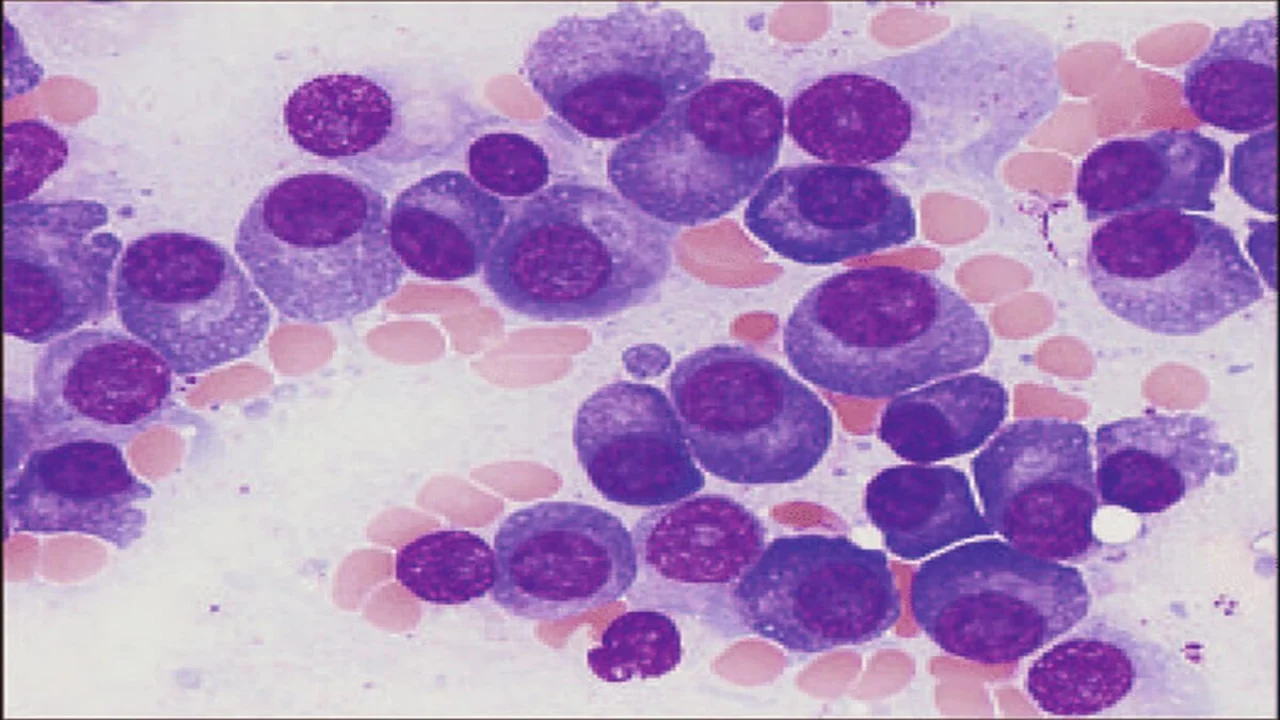
Multiple Myeloma: Early Death Common and Preventable
Improved survival among patients with multiple myeloma is one of the most impressive cancer treatment success stories in recent years.
A decade ago, patients survived an average 3 to 4 years following a multiple myeloma (MM) diagnosis, but median survival times have doubled and continue to improve, said multiple myeloma researcher Shaji Kumar, MD, of Mayo Clinic, Rochester, Minnesota.
This is due largely to the introduction of novel biologic therapies and greater use of autologous stem cell transplant. While there is still no cure for the neoplastic plasma-cell disorder, these treatments now routinely prolong initial remission and survival.
Early death remains common
Considered a rapidly fatal disease just a decade ago, MM is now considered more of a chronic condition for many, but not all, patients, Kumar said in a telephone interview.
Early death remains a significant and under-recognized problem in multiple myeloma, especially among patients with serious comorbidities or those who are very old. These patients often do not receive today’s gold-standard treatments, and that is a problem, Kumar said.
“About a quarter of patients will die within the first 2 to 3 years of diagnosis, for a number of reasons,” Kumar said, adding that he believes early mortality among multiple myeloma patients could be reduced by a third or even half if strategies to identify and treat those most at-risk were systematically applied.”
“Do’s and Don’ts” in early treatment
These strategies were outlined by Kumar and colleagues from Mayo Clinic and the University of Alabama at Birmingham in a recent analysis, published ahead of print by the American Journal of Hematology.
“Multiple myeloma is not a rare disease, but it is not commonly seen by oncologists in general practice,” analysis co-author Luciano J. Costa, MD, of the University of Alabama at Birmingham said. “Some may see only 1 or 2 of these patients a year, so we felt it was important to highlight some key strategies for reducing early death rates in this population.”
In a separate population analysis of 30,324 multiple myeloma patients published late in 2014, Kumar, Costa and colleagues found that while early mortality–defined as death within a year of MM diagnosis–has decreased over time, it still occurred in 28.6% of patients diagnosed in the U.S. between 1993 and 2010.
The incidence of early death among patients diagnosed before the age of 65 was 17.6% and incidence among older patients was 35.3%.
Majority of MM patients are age 65+
“About two-thirds of patients are 65 or older when diagnosed, so this at-risk group represents the overwhelming majority of patients,” Costa said. “And most of these older patients are not dying from refractory disease.”
Instead, Costa said he believes many die because they are either not getting optimal therapies or because they are very ill from co-morbid diseases at the time of their diagnoses.
These very ill or elderly patients have typically been excluded from multiple myeloma clinical trials, so there is little to guide physicians treating them.
This is why careful risk stratification and identification of co-morbidities immediately following a MM diagnosis is critical, Kumar noted.
“We need to manage the myeloma in the context of the other things going on with the patient,” he said.
The strategy for managing newly diagnosed MM outlined by Costa, Kumar and colleagues included a series of “do’s” and “don’ts” derived from their experience treating patients with the bone marrow cancer. Their aim was not to present comprehensive recommendations for treatment, but, instead, to focus on strategies designed to avoid early complications and death.
Among the recommended “do’s” and “don’ts”:
Do institute prompt systemic therapy
The researchers’ 2014 analysis revealed that the risk of early death was higher when novel MM drugs were not used as part of treatment.
While physicians may be tempted to focus on supportive care for conditions that accompany MM, such as hypercalcemia, bone lesions, renal failure and anemia, the researchers wrote that these treatments should not replace systemic therapy.
“It is crucial to keep in mind that ultimate symptom control or reversal of complication can only be obtained with systemic treatment, and none of the supportive measures above precludes prompt initiation of systemic therapy,” they wrote.
Do treat hypercalcemia aggressively
Approximately 1 in 5 patients develop hypercalcemia, resulting from increased activation of osteoclasts. The researchers noted that the “prompt and effective management of hypercalcemia is imperative to prevent early mortality in newly diagnosed MM.”
They added that in cases of mild hypercalcemia, aggressive rehydration with normal saline along with corticosteroids should suffice, as long as hydration is carefully monitored to avoid congestive heart failure.
In moderate to severe cases (serum calcium >12 mg/dL), an ECG is recommended to rule out arrhythmias. In addition to hydration and corticosteroids, the researchers recommended anti-bone resorption therapies, and they noted that results from two separate trials in patients with malignancy-related hypercalcemia found zoledronic acid to be superior to pamidronate for normalizing calcium levels.
Drugs that cause hypercalcemia should also be avoided, as well as drugs that can worsen neurological status in the setting of concurrent hypercalcemia, “to allow adequate assessment of neurological status.”
Do avoid and manage infections
Infections are the most common cause of early death in MM patients. One study found that 45% of deaths within 2 months of diagnosis were associated with infections. A population-based study from Sweden showed a 7- to 10-fold increase in bacterial and viral infection risk in MM patients, compared to the general population.
The use of prophylactic antibiotics to prevent infections in MM remains controversial, and the researchers noted that routine prophylaxis is not advised. They did, however, recommend the use of TMP-SMX to prevent fungal pneumonias in patients treated with 20 mg/d or more of prednisone. They also recommended prophylactic use of acyclovir or valacyclovir for patients receiving proteasome inhibitors (PIs) that disrupt normal T-cell immunity.
“For all patients receiving bortezomib and for that matter even newer PIs such as carfilzomib, we recommend administering antiviral prophylaxis with acyclovir 400 mg twice daily or valacyclovir 500 mg once a day,” they wrote.
Do avoid thromboembolic events (VTE)
This risk increases with age, and patients with blood cancers such as MM have an especially high risk for clot-related events. The researchers recommend educating all newly diagnosed patients on the warning signs for the development of VTEs. They also recommend the use of VTE prophylaxis in all newly diagnosis MM patients receiving IMiD-immunomodulator therapies.
“In MM patients who develop a thrombosis upon initiating treatment, it is reasonable to hold their treatment and resume after they are therapeutically anticoagulated,” the researchers wrote. “This level of anticoagulation may be continued for the remainder of the duration of MM-directed therapy as long as the risk of serious bleeding complications is deemed acceptable.”
Remaining “do’s” and “don’ts” recommended in the analysis included:
- Do address comorbidities and manage pain.
- Don’t postpone systemic therapy to address localized lesions.
- Don’t administer prolonged courses of high-dose corticosteroids.
- Don’t change well-tolerated therapy due to perceived suboptimal response if clinical benefit is shown.
- Don’t administer radiation when symptoms can be managed with systemic therapy.
- Don’t administer inferior treatment solely based on advanced age of performance status.
“In recent years we have seen an explosion in the number of available therapies for multiple myeloma, but older, sicker patients may not be getting these treatments,” Costa said. “Since about two-thirds of newly diagnosed patients are age 65 or older, it is important to address the issue of suboptimal treatment in this population.”
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
- Last updated by Dayyal Dungrela, MLT, BSc, BS
Cite this page:
- Comment
- Posted by Salynn Boyles