Blood Group Systems
Discover an in-depth analysis of various blood group systems, including Lewis, Kell, Duffy, and Kidd, with a focus on their antigens, antibodies, and clinical relevance to transfusions and disease resistance.
The International Society of Blood Transfusion (ISBT) has categorized red blood cell antigens into 25 distinct blood group systems. A blood group system is defined by the red cell antigens produced by alleles, which are alternative forms of a gene, located at a specific gene locus or at closely related loci.
Blood group genes follow Mendelian inheritance and are primarily located on autosomes. Notably, most blood group genes exhibit co-dominance, meaning that both allelic forms are expressed equally in individuals with heterozygous gene pairs, without one gene being dominant over the other. The specific alleles present at a gene locus determine an individual's genotype, while the phenotype represents the outward expression of this genotype.
In blood transfusion practices, the ABO and Rh blood group systems are of paramount importance. This is because the A, B, and Rh D antigens are the most immunogenic, meaning they can trigger a strong antibody response. The presence of alloantibodies against these antigens can result in the destruction of transfused red blood cells or lead to hemolytic disease of the newborn (HDN). Additionally, ABO antigens are crucial in organ transplantation.
ABO Blood Group System
The ABO system classifies blood into four main groups: A, B, AB, and O. These groups are identified based on the presence or absence of A and/or B antigens on the surface of red blood cells. Landsteiner’s Law states that individuals lacking a specific antigen on their red blood cells will naturally have antibodies against that antigen in their plasma (Table 2). The ABO system is unique in that the absence of an antigen always corresponds with the presence of its respective antibody in the plasma.
There is geographical variation in the distribution of ABO blood groups, but overall, the O blood group tends to be the most common globally, while the AB group is the least common. This variation highlights the significance of the ABO system in both medical and population genetics contexts.
| Blood Group | System |
|---|---|
| ABO | Dombrock |
| MNS | Colton |
| P | Landseiner-Weiner |
| Rh | Chido/Rogers |
| Lutheran | Hh |
| Kell | Kx |
| Lewis | Gerbich |
| Duffy | Cromer |
| Kidd | Knops |
| Diego | Indian |
| Yt | Ok |
| Xg | Raph |
| Scianna | - |
| Blood group | Caucasian frequency | Indian frequency | Genotype | Antigen(s) on red cells | Antibody in plasma |
|---|---|---|---|---|---|
| A | 40% | 27% | AA or AO | A | Anti-B |
| B | 11% | 31% | BB or BO | B | Anti-A |
| AB | 4% | 8% | AB | AB | Nil |
| O | 45% | 34% | OO | Nil | Anti-A and Anti-B |
| Note: The ABO genes follow a pattern of dominance, where A and B genes are dominant, and the O gene is recessive. Individuals with AA, BB, and OO genotypes are homozygous for A, B, and O blood groups, respectively, while AO, BO, and AB individuals are heterozygous. | |||||
Blood Group O
Blood Group O is typically the most prevalent blood type among populations. Individuals with this blood group have red cells that exhibit high levels of H antigen on their surface. The genotype for this group is OO, and their plasma contains antibodies against both A and B antigens, namely anti-A, anti-B, and anti-A,B. These antibodies are predominantly IgG, which can cross the placenta, potentially leading to hemolytic disease of the newborn.
Blood Group A
Individuals with Blood Group A possess either the genotype AA or AO. Their red cells display A and H antigens, while their plasma contains anti-B antibodies, primarily IgM in nature. This group is further divided into two subgroups: A1 (80%) and A2 (20%). Some individuals from the A2 or A2B groups can produce weak anti-A1 antibodies, which generally do not cause clinical issues, but may interfere with blood grouping. The lectins from Dolichos biflorus can be used to distinguish between A1 and A2 red cells by agglutinating only A1 cells.
Blood Group B
For those with Blood Group B, the genotype is either BB or BO, and their red cells present B and H antigens. Their plasma contains anti-A antibodies, which are primarily IgM.
Blood Group AB
Blood Group AB is the rarest among the ABO types. Individuals with this blood group have the genotype AB, and their red cells display A, B, and small amounts of H antigens. This blood group is further categorized into A1B and A2B. Unlike other blood groups, individuals with AB blood do not possess anti-A or anti-B antibodies in their plasma.
Antigens of the ABO system
The ABO blood group system involves several antigens, including A (A1 and A2), B, and H, which are either glycolipids, glycoproteins, or glycosphingolipids. These antigens are found not only on red cells but also on white blood cells, platelets, and various body tissues. Additionally, they can be present in body secretions in individuals who are classified as secretors.
Distribution of ABH antigens:
- Red blood cells
- White blood cells (weak)
- Platelets (weak)
- Body tissues
- Body fluids (in secretors)
ABO antigens are weakly expressed at birth but gradually strengthen, reaching full expression by around one year of age. As individuals age, these antigens may become slightly less pronounced.
Formation of ABH Antigens
The H gene, with genotypes HH or Hh, produces a transferase enzyme that modifies precursor substances on red cells to form H substance. From there, the A and B genes on chromosome 9 produce enzymes that convert H substance into A and B antigens, respectively. For the A antigen, N-acetylgalactosamine is added to the H antigen chain, while for the B antigen, galactose is added.
However, some individuals inherit an inactive O gene, which produces no functional transferase, allowing the H antigen to remain unchanged, characterizing Blood Group O.

Bombay Phenotype
In rare cases, individuals do not inherit the H gene (genotype hh) and are unable to synthesize H substance, preventing them from expressing A or B antigens, even if they inherit the corresponding genes. These individuals have the Bombay blood group or Bombay phenotype (Oh), a rare blood group first discovered in Bombay, India. People with this phenotype lack H, A, and B antigens on their red cells due to the lack of H (and Se) genes, and their plasma contains strong anti-H antibodies, in addition to anti-A and anti-B. As a result, Bombay phenotype individuals can only receive blood from other Bombay phenotype donors.
Identification of Bombay Phenotype
- Blood group: O
- Cross-matching: Serum incompatible with O cells
- Red cells yield negative reaction with anti-H lectin
Secretors and Non-secretors
Secretors are individuals who release A, B, and H antigens into various bodily fluids, including plasma, gastric juice, saliva, sweat, tears, semen, and milk. This ability is governed by the presence of a dominant secretor gene (Se) located on chromosome 19. Approximately 80% of the population are secretors, possessing either the genotype Sese or SeSe, while the remaining 20% are classified as non-secretors with the genotype sese. Both secretors and non-secretors exhibit ABO blood group antigens on their red blood cells.
The specific antigens secreted into body fluids vary according to the individual’s ABO blood group:
- Group A: A and H antigens
- Group B: B and H antigens
- Group AB: A, B, and H antigens
- Group O: H antigen
These antigens found in body fluids are collectively referred to as ABH substances. Testing for these substances in saliva can help clarify cases where blood group typing is inconclusive.
The determination of secretor status in body fluids like saliva and semen is crucial in resolving discrepancies in ABO blood group typing. Additionally, this method plays an important role in forensic investigations, such as in cases of sexual assault where semen samples are analyzed to match ABH antigens with the ABO blood group of a suspect. The detection of soluble blood group antigens in secretions is done using inhibitor tests. In this test, if a soluble antigen is present in the saliva, the addition of its corresponding antibody will neutralize the antibody’s activity. Consequently, when red cells carrying the appropriate antigens are added to the sample, there will be inhibition of agglutination, indicating that the person is a secretor. On the other hand, if agglutination occurs, the individual is identified as a non-secretor.
For example:
- Blood group: B
- Saliva + Anti-B → Add B cells: No agglutination
- Interpretation: Secretor
- Blood group: O
- Saliva + Anti-A → Add A cells: Agglutination
- Saliva + Anti-B → Add B cells: Agglutination
- Saliva + Anti-H → Add O cells: No agglutination
- Interpretation: Secretor
- In non-secretors, the absence of soluble antigens allows the antibodies in the reagent to bind to red cells, leading to agglutination.
Antibodies of the ABO System
The most significant antibodies in blood transfusions are anti-A and anti-B, which are considered naturally occurring antibodies. These antibodies develop without prior exposure to foreign red blood cells containing the corresponding antigens. They are regularly present when the corresponding antigen is absent. However, they are not detectable in newborns due to the immaturity of their immune systems and typically appear around three to six months of age. It is believed that these antibodies are produced in response to A- and B-like antigens found in certain bacteria within the intestines and various foods. If anti-A or anti-B antibodies are detected in a newborn, they are usually of maternal origin, belonging to the IgG class.
Most naturally occurring anti-A and anti-B antibodies are of the IgM class. IgM antibodies are large molecules capable of binding up to ten antigens, which allows them to cause direct agglutination of red blood cells. These antibodies can effectively activate the complement system, leading to significant consequences, such as:
- Hemolytic transfusion reactions when ABO-incompatible blood is transfused.
- Acute graft rejection following an ABO-incompatible organ transplant.
- Hemolysis of donor red cells after ABO-incompatible bone marrow transplantation.
In rare cases, certain individuals—particularly those with blood group O—may develop a high concentration of ABO antibodies following immune stimulation through transfusion, pregnancy, or exposure to vaccines or bacterial antigens. These antibodies, usually of the IgG class, cannot be neutralized by soluble antigens in body fluids. Transfusion of blood from such individuals to recipients with blood group A or B can lead to severe hemolysis, making it inadvisable to consider group O donors as universal donors. In addition to causing hemolytic transfusion reactions, IgG antibodies can cross the placenta, leading to hemolytic disease of the newborn.
Concepts of Universal Donor and Recipient
Group O individuals have red blood cells that lack A and B antigens, preventing agglutination by anti-A or anti-B antibodies. For this reason, group O donors have traditionally been viewed as universal donors, while group AB individuals are considered universal recipients. However, this view is somewhat simplistic as it only accounts for the interaction between the recipient’s plasma and the donor’s red cells. In reality, the donor’s plasma may contain antibodies capable of destroying the recipient’s red cells. Additionally, antigens other than A, B, or RhD can trigger immune responses in the recipient.
The Rh System
The Rh system, named after the Rhesus monkey, was initially identified by Landsteiner and Weiner in 1940. They injected Rhesus monkey red blood cells into rabbits and guinea pigs, which produced antibodies that reacted with both Rhesus monkey cells and human red cells in 85% of the population (specifically white individuals in New York). This antigen was termed the Rh factor. Although later research revealed that the antibody they identified differed from the anti-D antibody discovered afterward, the term "Rhesus" remained in use. Additionally, Levine and Stetson are credited with independently discovering, in 1939, the anti-D antibody responsible for hemolytic disease of the newborn, further expanding our understanding of the Rh system.
The Rh system is second only to the ABO system in terms of importance in transfusion practices. Its significance lies in the immunogenicity of the Rh D antigen, which induces anti-D antibody production in 50-70% of Rh D-negative individuals. These antibodies can lead to hemolytic transfusion reactions and, in pregnant women, Rh hemolytic disease in the newborn.
The Rh system was independently discovered by Stetson and Levine in 1939, and by Landsteiner and Weiner in 1940.
Antigens of the Rh System
The Rh system is highly complex, comprising approximately 40 antigens. The most clinically significant antigens are C, D, E, c, and e, while an antigen labeled "d" does not actually exist. Among these, the D antigen is the most immunogenic, meaning it has the greatest capacity to elicit an immune response. There are several nomenclature systems for describing Rh antigens, with the Fisher-Race and Weiner systems being the most widely used.
According to the Fisher-Race system, three closely linked genes are inherited together on a single chromosome (haplotype) from each parent. The allelic forms of these genes are C and c, D and d, and E and e, resulting in eight possible haplotypes: Cde, cde, cDE, cDe, cdE, Cde, CDE, and CdE. Since one haplotype is inherited from each parent, 36 genotypes are possible, such as Cde/cde, Cde/cDe, and CDE/cde. If the D antigen is present in either a homozygous (D/D) or heterozygous (D/d) form, the individual is considered Rh positive, while Rh negative individuals are homozygous for the d allele (d/d). The "d" gene was once thought to be an amorph, or a nonfunctional gene.
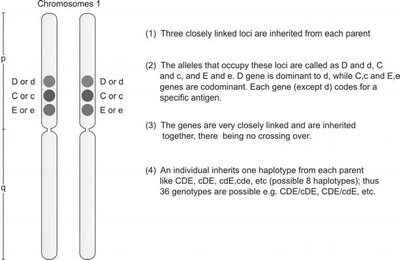
According to Dr. Alexander Weiner’s theory, each individual inherits a single Rh gene from each parent, but this gene has multiple alleles (Figure 3). The Weiner system, which utilizes the Rh-Hr nomenclature, differs from the Fisher-Race system. Fisher-Race suggests that three closely linked genes are passed down from each parent, while Weiner’s theory proposes that a single gene with several alleles is inherited from both parents.

Current genetic studies indicate that both the Fisher-Race and Weiner systems hold partial accuracy. Research has demonstrated that the RH locus is located on chromosome 1, consisting of two closely linked genes: RHD and RHCE (Figure 4). The alleles of the RHCE gene are represented as CE, Ce, ce, and cE.

In Rh-negative individuals, genetic variations such as deletions, point mutations, or partial mutations in the D gene have been identified. Unlike ABO antigens, Rh antigens are exclusive to red blood cells and are not secreted in bodily fluids. Additionally, Rh antigens are fully expressed on fetal red blood cells, even before birth.
Based on the presence or absence of the D antigen on red blood cells, an individual is categorized as Rh-positive (when the D antigen is present) or Rh-negative (when the D antigen is absent). The frequency of D antigen expression differs across populations. For example, approximately 95% of the Indian population is Rh D positive, while only 5% are Rh D negative. In Caucasians, about 85% are Rh positive, while 15% are Rh negative.
Various forms of the D antigen, such as weak D and partial D, also exist (Figure 5). Red blood cells that exhibit weak D antigen were previously referred to as Du cells, as they weakly react with anti-D reagents. In these cases, there is a reduced number of D antigen sites on the cells. Individuals with Du cells do not produce anti-D antibodies following stimulation from D antigen, such as after receiving D-positive blood. Du donors, however, are considered Rh positive, and their blood should not be given to Rh-negative individuals.
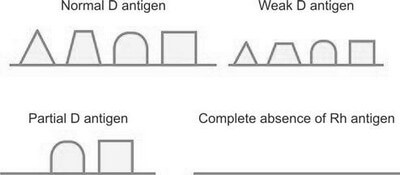
For individuals with partial D antigen, certain portions of the D antigen may be absent. Variants of the partial D antigen exist, and individuals with the DVI variant can produce anti-D antibodies against the missing antigen segments. In clinical practice, such individuals are considered Rh negative, although they are typically recognized after they have already developed anti-D antibodies. As donors, individuals with partial D are treated as Rh positive.
A rare condition, Rh null, involves the complete absence of Rh antigens on red blood cells. This condition is associated with stomatocytosis and compensated hemolysis.
Rh Antibodies
Most Rh antibodies are generated through immune responses, usually triggered by blood transfusions or pregnancy. These antibodies are predominantly of the IgG class.
Rh antibodies can lead to hemolytic transfusion reactions or hemolytic disease of the newborn (HDN). Since Rh antibodies do not activate complement, hemolysis occurs extravascularly, mainly within the spleen. Due to the highly immunogenic nature of the D antigen, Rh-negative individuals, particularly women of childbearing age, should only receive Rh-negative blood. During pregnancy, IgG anti-D antibodies can cross the placenta, resulting in hemolysis of fetal red cells and causing Rh hemolytic disease in the newborn. Administering Rh immune globulin to Rh-negative women during mid-pregnancy and within 72 hours after delivery can prevent this condition. While anti-D and anti-c antibodies can cause severe HDN, anti-C, anti-E, and anti-e antibodies either do not cause HDN or only result in mild cases.

Other Blood Group Systems
While the ABO and Rh blood group systems are the most well-known, several other blood group systems are clinically significant. These lesser-known systems are important in specific clinical contexts, such as transfusions and disease susceptibility. Below is a summary of other blood group systems beyond ABO and Rh.
| Blood Group System | Antigens | Antibodies | Comments |
|---|---|---|---|
| Lewis | Lea, Leb | Natural, IgM | Lewis antigens are passively absorbed onto red cells from plasma. Lewis antibodies are typically of little clinical significance. |
| Kell | About 20 (KEL1, KEL2, etc) | IgG | Anti-K antibodies can lead to hemolytic transfusion reactions and hemolytic disease of the newborn. Individuals lacking Kell precursors may exhibit shortened red cell lifespan and acanthocytic features, known as the MacLeod phenotype. |
| Duffy | Fya, Fyb | IgG | Duffy antibodies can cause hemolytic transfusion reactions. Notably, Plasmodium vivax uses the Duffy antigen site to invade red blood cells. Individuals with the Fy(a-b-) phenotype, common in Black populations, are resistant to P. vivax infection. |
| Kidd | JKa, JKb | IgG | Kidd antibodies are associated with delayed transfusion reactions and can contribute to mild hemolytic disease of the newborn. |
| MNSs | M, N, S, s | - | M and N antigens hold importance in paternity testing due to their genetic variability. |
| P | P, P1, Pk | IgM, IgG | Auto-anti-P antibodies are involved in paroxysmal cold hemoglobinuria, a rare autoimmune hemolytic disorder. |
These blood group systems, although less frequently discussed compared to ABO and Rh, play vital roles in transfusion medicine and immunohematology. For instance, antibodies against the Kell and Duffy antigens can provoke serious transfusion reactions or contribute to hemolytic disease of the newborn, underscoring the importance of compatibility in blood transfusions. Additionally, certain antigenic profiles, such as the Duffy Fy(a-b-) phenotype, offer protection against diseases like malaria, highlighting the connection between blood group antigens and disease resistance. Understanding these blood group systems is crucial for managing blood transfusions and recognizing immunological reactions associated with blood groups.
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Reference(s)
- Monica Cheesbrough. District Laboratory Practice in Tropical Countries. Part 1 and Part 2. Cambridge University Press, 1998.
- Lewis SM, Bain BJ, Bates I. Dacie and Lewis Practical Hematology. Churchill Livingstone, 2001, 9th, 978-0443063770.
Cite this page:
- Posted by Dayyal Dungrela