How Gut Bacteria May Shape Parkinson’s Disease
A large meta-analysis shows people with Parkinson’s disease have a distinct gut microbiome with reduced vitamin producing microbes and weakened protective metabolites, pointing to a possible gut driven pathway in the disease.
Parkinson’s disease is usually described as a brain disorder that affects movement, balance and daily activities. But in recent years, scientists have been looking somewhere unexpected for clues about this condition: the gut.
A large analysis of gut bacteria profiles from people with Parkinson’s disease and healthy individuals across several countries has revealed a distinct microbial “signature” in Parkinson’s patients. These findings support the idea that what happens in the gut may influence what happens in the brain.
A global look at the Parkinson’s gut microbiome
To move beyond small, local studies, researchers combined fecal shotgun sequencing data from multiple countries, including Japan, the USA, Germany, China and Taiwan. This kind of meta analysis strengthens patterns that are truly linked to disease and filters out random noise from small samples.
In total, data from 94 people with Parkinson’s disease and 73 healthy controls in Japan were analyzed together with international datasets. This allowed scientists to search for consistent microbiome changes across populations with different diets, lifestyles and genetics.
Microbial diversity in Parkinson’s disease: an unusual pattern
In many chronic conditions such as inflammatory bowel disease or obesity, patients tend to have lower gut microbial diversity compared with healthy people. Surprisingly, Parkinson’s disease appears to be different.
Increased α diversity in Parkinson’s
The study found that individuals with Parkinson’s disease showed increased α diversity, meaning they had a wider variety of bacterial species in their gut. This makes Parkinson’s stand out from the usual disease pattern of “less diverse microbiome equals poorer health.”
However, higher diversity does not automatically mean healthier. What matters is which bacteria are present, what they are doing, and how they interact with the host. In Parkinson’s disease, the mix of bacteria and their metabolic activities appear shifted in a way that may contribute to disease mechanisms.
Key bacterial winners and losers in Parkinson’s guts
When the researchers zoomed in on specific bacterial species, they found clear changes linked to Parkinson’s disease.
Increased Akkermansia muciniphila
One of the most notable microbes that increased in Parkinson’s patients was Akkermansia muciniphila. This species is known for its ability to digest mucus, the protective layer that lines the gut.
- At moderate levels, A. muciniphila is often considered beneficial.
- However, if its levels are too high, excessive mucus degradation could potentially alter the gut barrier and influence how immune cells react to gut contents.
In Parkinson’s disease, this increase raises questions about how the mucus layer and gut permeability might be affected.
Decreased Roseburia intestinalis and Faecalibacterium prausnitzii
Two important bacterial species were found to be decreased in people with Parkinson’s:
- Roseburia intestinalis
- Faecalibacterium prausnitzii
These bacteria are famous for producing short chain fatty acids (SCFAs), especially butyrate, which:
- Provide energy to colon cells.
- Help maintain the gut barrier.
- Support anti inflammatory immune responses.
Their reduction suggests a loss of protective, health promoting functions in the gut environment of Parkinson’s patients.
Metabolic changes: fewer SCFAs and polyamines
Gut bacteria are not just passive residents. They act like a large biochemical factory that produces a wide range of metabolites. In people with Parkinson’s disease, this factory seems to shift toward a less protective mode.
Reduced short chain fatty acids (SCFAs)
The study reported lower fecal levels of SCFAs in Parkinson’s patients. Because SCFAs support gut barrier integrity and regulate inflammation, their decline could have several implications:
- Weakened gut lining, allowing more potentially harmful molecules to interact with immune cells.
- Increased inflammatory signals that may reach the nervous system.
- Possible contribution to neuroinflammation, which is increasingly recognized as a factor in Parkinson’s disease.
Reduced polyamines
Levels of polyamines, another important group of microbial metabolites, were also reduced. Polyamines are involved in cell growth, membrane stability and cellular stress responses.
Together, reduced SCFAs and polyamines suggest a gut environment that is less supportive of tissue health and more prone to subtle, chronic disturbances.
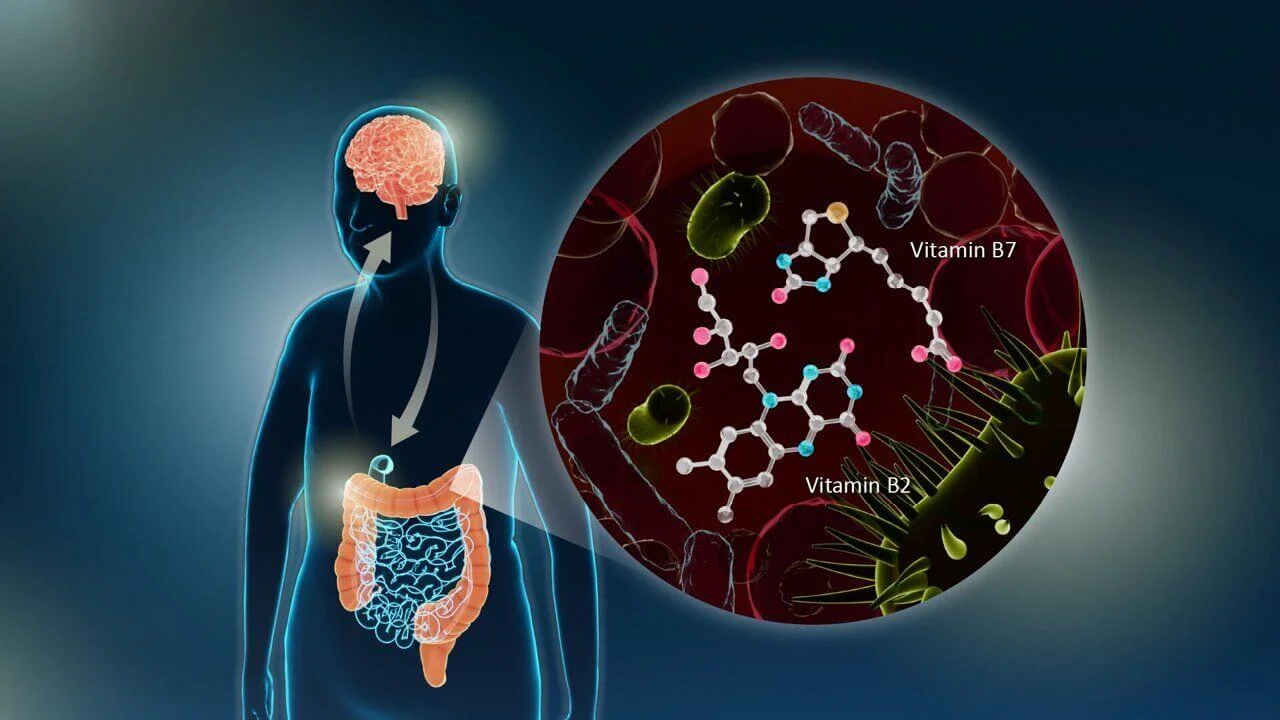
Vitamin pathways under pressure: riboflavin and biotin
Beyond individual bacteria and metabolites, the researchers examined the gene pathways present in the microbiome. This reveals what biochemical capacities the overall gut community has.
Downregulation of vitamin biosynthesis genes
The analysis showed a downregulation of genes involved in the biosynthesis of two key vitamins:
- Riboflavin (vitamin B2)
- Biotin (vitamin B7)
These vitamins are essential for multiple aspects of cellular energy production and nervous system function. Many gut bacteria contribute to the body’s pool of B vitamins, so a loss of these pathways in the microbiome may reduce the availability of these nutrients.
Why this matters for the brain
Riboflavin and biotin are important for:
- Mitochondrial energy metabolism.
- Proper functioning of neurons.
- Protection against certain types of cellular stress.
Their reduced biosynthesis in the gut environment points to a possible link between microbial vitamin production and neuronal health in Parkinson’s disease. This opens the door to exploring vitamin targeted therapies or microbiome based approaches as supportive strategies.
The gut brain connection in Parkinson’s disease
The findings provide strong support for a gut brain connection in Parkinson’s disease. Several mechanisms may be involved:
- Altered gut barrier and mucus layer
- Increased Akkermansia muciniphila suggests changes in mucus turnover.
- Combined with reduced SCFAs, this might compromise the gut barrier and increase exposure of the immune system to gut contents.
- Inflammation and immune activation
- Loss of SCFA producers like Roseburia intestinalis and Faecalibacterium prausnitzii reduces anti inflammatory signals.
- This can tilt the balance toward chronic, low grade inflammation, which may influence the nervous system.
- Nutrient and vitamin availability
- Reduced microbial production of riboflavin and biotin may affect neuronal resilience.
- This could contribute to vulnerability of specific brain regions involved in Parkinson’s disease.
While this research does not prove that gut changes cause Parkinson’s disease, it strongly suggests that the microbiome may help shape the course and possibly the onset of the condition.
Could diet and probiotics help in Parkinson’s disease?
Because the gut microbiome is strongly influenced by diet and lifestyle, these findings naturally raise the question of whether dietary interventions could help manage Parkinson’s disease.
Restoring beneficial bacteria
The reduction in SCFA producing bacteria points to strategies aimed at:
- Supporting Roseburia and Faecalibacterium populations.
- Promoting other butyrate and SCFA producers via dietary fibers and prebiotics.
While the study does not test specific interventions, it suggests that maintaining a microbiome rich in SCFA producers may be beneficial for gut and possibly brain health.
Vitamin focused approaches
The observed decrease in microbial genes for riboflavin and biotin biosynthesis hints that:
- Dietary vitamin support might help counterbalance reduced microbial production.
- Future research may explore whether targeted probiotics and vitamin supplementation can improve symptoms or slow progression.
At this stage, such ideas remain promising but unproven. Well designed clinical trials are needed before firm recommendations can be made.
Differences between countries: a complex microbiome puzzle
Interestingly, the study found that different bacterial species were linked to reduced riboflavin and biotin pathways in different countries.
This means:
- The overall functional shift in the microbiome can be similar across populations
- for example, less vitamin production
- yet the exact bacterial players responsible for that shift may vary.
- Factors such as diet, environment, genetics and medication use likely shape which species gain or lose ground in Parkinson’s disease.
This complexity shows why microbiome research often needs large, international datasets to distinguish universal patterns from regional variations.
What this means for the future of Parkinson’s research
The study offers several important messages for future research and for how we think about Parkinson’s disease.
Reinforcing the gut brain axis
The results add weight to the concept that:
- The gut microbiome is not just a bystander but may be actively involved in Parkinson’s mechanisms.
- Changes in gut bacteria and their metabolites could contribute to neuroinflammation, nutrient availability and gut barrier function.
New directions for therapy
Potential future strategies suggested by the findings include:
- Microbiome targeted approaches
- Probiotics or prebiotics to support SCFA producers and balance species such as Akkermansia.
- Diets that nourish beneficial bacteria and enhance metabolite profiles.
- Nutritional and vitamin based approaches
- Addressing possible deficits in riboflavin and biotin production.
- Combining dietary changes with other medical treatments.
- Personalized medicine
- Accounting for country specific and individual microbiome differences.
- Using microbiome signatures as biomarkers to help track disease or response to therapy.
Need for larger and longer studies
The authors emphasize that larger, more extensive studies are essential to:
- Confirm these microbiome patterns in diverse populations.
- Test whether changing the microbiome can truly affect symptoms or progression.
- Develop safe and effective microbiome based interventions for clinical use.
Take home message for the general public and science lovers
Parkinson’s disease is not only a story of damaged brain cells. It may also be a story written in the trillions of microbes living in the gut.
Researchers found that:
- People with Parkinson’s disease have higher overall gut bacterial diversity, but with specific harmful shifts.
- Beneficial SCFA producing bacteria such as Roseburia intestinalis and Faecalibacterium prausnitzii are reduced.
- Metabolites like SCFAs and polyamines are lower, potentially affecting gut health and inflammation.
- Genes involved in making riboflavin and biotin are less active, hinting at a connection between gut vitamin production and neuronal health.
- These patterns support a strong gut brain link, pointing toward new research on diet, microbiome modulation and targeted vitamin support in Parkinson’s disease.
For now, these discoveries mainly guide scientists toward new hypotheses and clinical trials. For patients and families, they highlight a hopeful idea: understanding and gently guiding the invisible world of gut microbes may one day become part of how we prevent or manage Parkinson’s disease.
The research was published in npj Parkinson’s Disease on May 21, 2024.
This article has been fact checked for accuracy, with information verified against reputable sources. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
- Last updated by Dayyal Dungrela, MLT, BSc, BS
Reference(s)
- Nishiwaki, Hiroshi., et al. “Meta-analysis of shotgun sequencing of gut microbiota in Parkinson’s disease.” npj Parkinson’s Disease, vol. 10, no. 1, 21 May 2024, doi: 10.1038/s41531-024-00724-z. <https://www.nature.com/articles/s41531-024-00724-z>.
Cite this page:
- Posted by Heather Buschman