Physical Examination of Urine
Physical examination of urine includes description of color, odor, clarity, volume, and specific gravity. Urinalysis continues to be a powerful tool in obtaining crucial information for diagnostic purposes in medicine. Learn more.

Urine serves as a valuable medium for uncovering both physical and biochemical irregularities within the body. Its examination plays a pivotal role in screening and diagnosing various conditions, including urinary tract infections, kidney disorders, liver issues, diabetes, and diverse metabolic conditions. However, prior to delving into the examination process, it is crucial to assess the specimen's acceptability.
Several key parameters are scrutinized during the physical examination of urine, each offering unique insights into the individual's health status:
- Volume: The quantity of urine expelled.
- Color: The hue, which may indicate different metabolic processes.
- Appearance: The overall clarity or turbidity of the urine.
- Odor: Unveiling distinct scents associated with specific conditions.
- Specific Gravity: Reflecting the concentration of solutes in the urine.
- pH: Measuring the acidity or alkalinity of the urine.
Volume
Accurate measurement and assessment of urine volume, specifically from the 24-hour specimen, are pivotal in unraveling essential insights into an individual's renal health. The typical range for 24-hour urinary output in adults spans from 600 to 2000 ml, with fluctuations influenced by factors such as fluid intake, dietary habits, and environmental conditions.
Key Abnormalities in Urinary Volume
- Polyuria:
- Definition: Excessive urinary volume surpassing 2000 ml/24 hours.
- Associated Conditions:
- Diabetes Mellitus: Linked to osmotic diuresis.
- Diabetes Insipidus: Stemming from the inadequate secretion of antidiuretic hormone.
- Chronic Renal Failure: Characterized by a diminished concentrating ability of the kidneys.
- Diuretic Therapy: Influencing fluid balance.
- Oliguria:
- Definition: Reduced urinary volume falling below 400 ml/24 hours.
- Causes:
- Febrile States: Elevated body temperature impacting renal function.
- Acute Glomerulonephritis: Marked by decreased glomerular filtration.
- Congestive Cardiac Failure: Reflecting compromised cardiac output.
- Dehydration: Resulting from diminished renal blood flow.
- Anuria:
- Definition: Scant urinary output, measuring less than 100 ml/24 hours, or a complete cessation of urine flow.
- Occurrence:
- Acute Tubular Necrosis: Evident in conditions like shock or hemolytic transfusion reactions.
- Acute Glomerulonephritis: Signifying a severe renal impairment.
- Complete Urinary Tract Obstruction: Leading to a halt in urine excretion.
Color
In its natural state, fresh urine typically exhibits a pale yellow or amber hue, attributed to a combination of pigments collectively referred to as urochrome. This normal coloration provides valuable insights into an individual's hydration status, ranging from colorless urine indicative of overhydration to dark yellow hues signaling dehydration.
The spectrum of urine colors extends beyond the norm, encompassing various abnormal hues linked to specific health conditions, as outlined in Table 1. This table serves as a comprehensive reference, shedding light on abnormal urine colors and their associated medical contexts.
| Colors | Conditions |
|---|---|
| Colorless | Dilute urine (diabetes mellitus, diabetes insipidus, overhydration) |
| Red | Hematuria, Hemoglobinuria, Porphyria, Myoglobinuria |
| Dark brown or black | Alkaptonuria, Melanoma |
| Brown | Hemoglobinuria |
| Yellow | Concentrated urine |
| Yellow-green or green | Biliverdin |
| Deep yellow with yellow foam | Bilirubin |
| Orange or orange-brown | Urobilinogen/Porphobilinogen |
| Milky-white | Chyluria |
| Red or orange fluorescence with UV light | Porphyria |
| Note: Many drugs cause changes in urine color; drug history should be obtained if there is abnormal coloration of urine. | |
Appearance
Normal urine, when freshly voided, possesses a clear and transparent appearance. Various factors leading to cloudy or turbid urine are detailed in Table 2. Foamy urine may manifest in situations marked by elevated protein or bilirubin levels, offering insights into potential health indicators. Understanding these visual aspects aids in the assessment of urine characteristics and potential underlying conditions.
| Cause | Appearance | Diagnosis |
|---|---|---|
| Amorphous phosphates | White and cloudy on standing in alkaline urine | Disappear on the addition of a drop of dilute acetic acid |
| Amorphous urates | Pink and cloudy in acid urine | Dissolve on warming |
| Pus cells | Varying grades of turbidity | Microscopy |
| Bacteria | Uniformly cloudy; do not settle at the bottom following centrifugation | Microscopy, Nitrite test |
Odor
The scent of freshly voided urine is characterized by a typical aroma, owing to the presence of volatile organic acids. Upon standing, a shift occurs, and the odor transitions to an ammoniacal scent, a result of bacterial decomposition of urea into ammonia. Various abnormal odors may be indicative of specific conditions, including:
- Fruity Odor: Linked to ketoacidosis and periods of starvation.
- Mousy or Musty Odor: Associated with Phenylketonuria.
- Fishy Odor: Indicates urinary tract infection with Proteus or tyrosinaemia.
- Ammoniacal Odor: Found in urinary tract infections with Escherichia coli or in old, stagnant urine.
- Foul Odor: Suggestive of a urinary tract infection.
- Sulfurous Odor: Identified in cases of Cystinuria.
Specific Gravity (SG)
Urine specific gravity, often referred to as relative mass density, is a measure influenced by the concentration of solutes in the urine. Think of it as a comparison between the density of urine and distilled water at a specific temperature. The baseline for distilled water is 1.000.
In normal urine, the specific gravity typically falls between 1.003 to 1.030, with variations linked to hydration levels. This metric is closely tied to urea and sodium concentrations. As the solute levels go up, so does the specific gravity, and it decreases with a rise in temperature due to the expansion of volume.
The specific gravity of urine serves as a gauge for the kidneys' ability to concentrate. However, it can be influenced by the presence of proteinuria and glycosuria.
Understanding Changes in Specific Gravity
- Increased Specific Gravity:
- Diabetes mellitus (glycosuria)
- Nephrotic syndrome (proteinuria)
- Fever
- Dehydration
- Decreased Specific Gravity:
- Diabetes insipidus (consistently between 1.002-1.003)
- Chronic renal failure (fixed at 1.010 due to tubular concentrating loss)
- Compulsive water drinking
Methods of Measurement
Various methods, such as the urinometer, refractometer, and reagent strip, are employed to measure specific gravity, providing valuable insights into the composition of urine.
Urinometer method
This way of measuring things relies on how liquids can push things up. We use a tool called a urinometer (which is like a special float) in a container filled with urine (see Figure 1A). If there's a lot of stuff in the urine, the urinometer floats higher (high SG). If there's not much stuff, it sinks more into the urine (low SG).
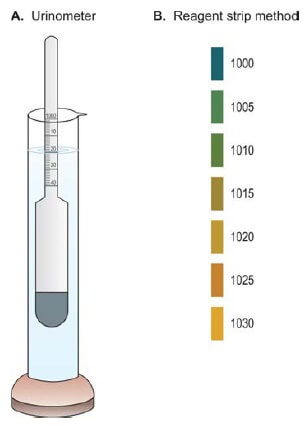
To make sure a urinometer is right, we check it with distilled water. In distilled water, the urinometer should read 1.000 at the calibration temperature. If it doesn't, we need to adjust future test readings accordingly.
Here's how you do it:
- Pour 50 ml of urine into a measuring cylinder.
- Gently put the urinometer into the urine and let it float freely.
- Wait for the urinometer to settle without touching the sides or bottom of the cylinder.
- Read the specific gravity (SG) on the scale at the surface of the urine (the lowest point of the curved surface).
- Take out the urinometer and quickly check the temperature of the urine using a thermometer.
Adjusting for Temperature: The density of urine changes with temperature, which can give a wrong specific gravity (SG) reading. To fix this, check the calibration temperature of the urinometer. For every 3°C above the calibration temperature, add 0.001 to the SG reading. Subtract 0.001 for every 3°C below the calibration temperature.
Handling Dilution: If there's not enough urine for an SG measurement, you can dilute it appropriately. Multiply the last two digits of the SG by the dilution factor.
Dealing with Abnormal Solute Concentration: High SG due to glycosuria or proteinuria doesn't truly reflect kidney function. To fix this, subtract 0.003 from the temperature-adjusted SG for each 1 gm of protein/dl in urine and 0.004 for every 1 gm of glucose/dl in urine.
Refractometer method:
You can accurately find the specific gravity (SG) using a refractometer. This device measures how much light is bent as it passes through the dissolved stuff in the urine. The more stuff in the urine, the more the light bends, indicating a higher SG. This method is easy – just use 1-2 drops of urine. The result is shown on a scale or a digital display.
Reagent strip method
The reagent strip (see Figure 1B) checks how many ions are in your urine, and this relates to the specific gravity (SG). As the strength of ions in urine changes, a special material called a polyelectrolyte also changes. This alters the color of a pH indicator (bromothymol blue) on the strip.
Reaction and pH
pH measures how acidic or alkaline something is (acidic if pH is less than 7.0, alkaline if more than 7.0, neutral if 7.0). When urine sits, it turns alkaline due to losing carbon dioxide and making ammonia. So, it's best to check pH with fresh urine.
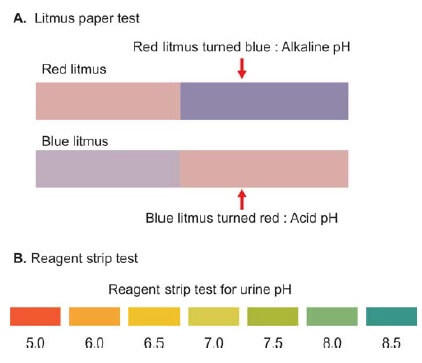
There are different ways to check urine pH: using litmus paper, pH indicator paper, a pH meter, or reagent strip tests.
- Litmus paper test: Dip a small strip of litmus paper in urine and note any color change. Blue turning red means acid urine, and red turning blue means alkaline urine (see Figure 2A).
- pH indicator paper: Dip the reagent area of the strip in urine, and compare the color change with the guide provided. This gives an approximate pH.
- pH meter: Dip the pH meter electrode in urine, and read the pH directly from the digital display if you need an exact value.
- Reagent strip test: The test area (see Figure 2B) releases H+ ions, changing the color of the pH-sensitive dye when it reacts with cations in urine.
The normal pH range for urine is 4.6 to 8.0, with an average of 6.0, which is slightly acidic. The pH of urine depends on your diet, acid-base balance, water balance, and how well your kidney tubes function.
Acidic urine can be found in conditions like ketosis (seen in diabetes, starvation, and fever), urinary tract infections caused by Escherichia coli, and with a high protein diet. On the other hand, alkaline urine can result from infections by bacteria like Proteus or Pseudomonas that turn urea into ammonia, severe vomiting, a vegetarian diet, old ammonia-containing urine samples, and chronic kidney failure.
Checking urine pH helps identify different crystals in urine. Adjusting urine pH can be useful in treating kidney stones (some stones form only in acidic urine, like uric acid stones; in such cases, urine is kept alkaline), urinary tract infections (keeping urine acidic is preferred), and in treatments involving specific drugs (like streptomycin, which works better in alkaline urine for urinary tract infections). In cases of unexplained metabolic acidosis, measuring urine pH helps diagnose renal tubular acidosis; with this condition, urine pH remains consistently alkaline despite metabolic acidosis.
The information on this page is peer reviewed by a qualified editorial review board member. Learn more about us and our editorial process.
Last reviewed on .
Article history
- Latest version
Cite this page:
- Comment
- Posted by Dayyal Dungrela