Diagnosis of Acute Myelocytic Leukemia (AML) and Acute Lymphocytic Leukemia (ALL)
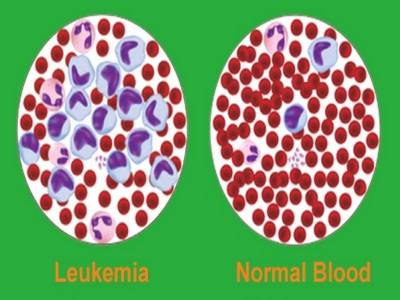
Leukemia is a malignant clonal hematopoietic stem cell disorders characterized by the rapid increase in the number of blast cells in the bone marrow and rapidly progressive fatal course if untreated. Acute leukemia (AL) are primary disorders of the bone marrow, also known as blood cancer.
What is acute leukemia?
It is defined as malignant clonal hematopoietic stem cell disorders characterized by the rapid increase in the number of blast cells in the bone marrow and rapidly progressive fatal course if untreated. Acute leukemia (AL) are primary disorders of the bone marrow, also known as blood cancer.
Classification of acute leukemias
The most widely used classification of acute leukemias is French-American-British (FAB) Co-operative Group classification. The FAB rule for the classification of acute leukemias was originally proposed in 1976. On the basis of the morphology and cytochemistry, they are classified into two major types.
- Acute myeloid leukemia (AML)
- Acute lymphoblastic leukemia (ALL)
Each type is further subclassified. See table 883.1
| Acute myeloid leukemia (AML) |
| M0: Acute myeloid leukemia, minimally differentiated |
| M1: Acute myeloid leukemia without maturation |
| M2: Acute myeloid leukemia, with maturation |
| M3: Acute promyelocytic leukemia M3v: Hypo- or microgranular promyelocytic leukemia |
| M4: Acute myelomonocytic leukemia M4Eo: Acute myelomonocytic leukemia with bone marrow eosinophilia |
|
M5: Acute monocytic leukemia
|
| M6: Acute erythroleukemia |
| M7: Acute megakaryocytic leukemia |
| Acute lymphoblastic leukemia (ALL) |
| L1: Lymphoblasts with constant, rounded nuclei, and adequate cytoplasm. Nucleoli are not prominent. |
| L2: More irregular lymphoblast and cytoplasm is available in large quantity. Nucleoli are large and may see one or more nucleoli. |
| L3: Large cells with moderate amount of deeply basophilic cytoplasm; prominent cytoplasmic vacuoles; regular nuclear membrane; 1-2 prominent nucleoli |
In contrast to French-American-British (FAB) classification, World Health Organization (WHO) classification recognizes AML with recurrent cytogenetic abnormalities, AML with multilineage dysplasia, and therapy-related AML as distinct entities.
Patients with clonal, recurrent cytogenetic abnormalities listed in Table 883.2 are considered to have AML irrespective of the percentage of blasts in blood or bone marrow. These patients have characteristic clinical and morphological features and a favorable response to therapy.
|
1. Acute myeloid leukemia with recurrent genetic abnormalities
|
|
2. Acute myeloid leukemia with multilineage dysplasia
|
|
3. AML and MDS, therapy related
|
|
4. AML, not otherwise categorized
|
Difference between Acute Myelocytic Leukemia (AML) and Acute Lymphocytic Leukemia (ALL)
| Characteristic Features | Acute Myelocytic Leukemia | Acute Lymphocytic Leukemia |
| Origin of cells | Myeloid series cells | Lymphoid series cells |
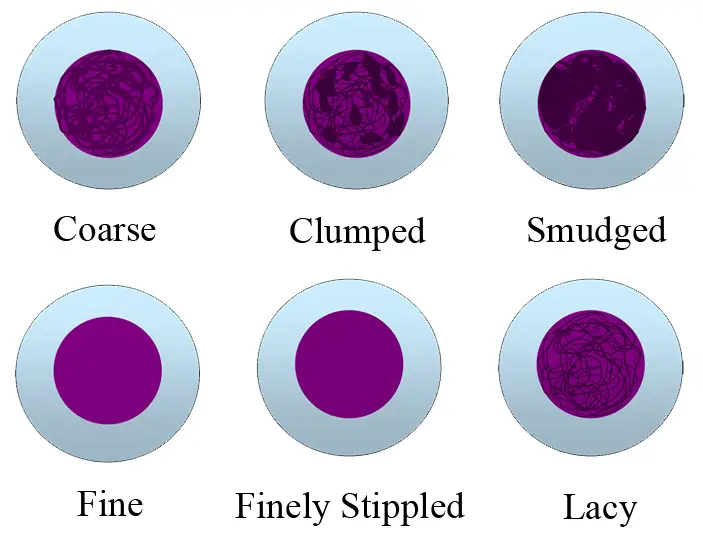
| Characteristics of blast cells | Cell is large in size with moderate cytoplasm. Chromatin patterns are fine and lacy. Nucleoli are prominent and are more than two. | Cell is small with scanty cytoplasm. Chromatin patterns are dense. Nucleoli are indistinct and are less than two. |
| Bone marrow | Mixed population of blast and myeloid cells. | Mainly blast cells and very few WBCs or RBCs |
| Sudan black and peroxidase | Positive | Negative |
| Auer rods | Present | Absent |
| Periodic Acid-Schiff (PAS) | Positive in Erythroblast in M6 leukemia | Positive (block patterns) in L1 and L2, and negative in L3 |
| Leukocyte Alkaline phosphatase (ALP) | Positive (It is used to differentiate CML from the leukemoid reaction) | Negative |
Sign and symptoms of acute leukemia
- Weakness and fatigue
- Low-grade fever
- Bone pain
- Bruising and mild bleeding from gums
- It appears suddenly
Diagnosis of acute leukemia
- This disease is most common in younger age group and more frequent in the children. Mostly found before the age of 20.
- Rapid development of anemia is most common with normocytic and normochromic red cells. You may see some nucleated red cells in the peripheral blood smear.
- Leucocytes (WBCs) count is variable. Mostly leucocytes count is less than 100000/μl.
- Thrombocytopenia (See also Morphology of Platelets)
• Petechiae and purpura may be seen in the skin and mucous membranes.
Laboratory findings in acute myelocytic leukemia (AML)
- Total leucocyte count (TLC) is variable. It is recorded that in 25% of patient's total leucocyte count is < 5000/μl, 25% of the patient has > 50000/μl and 5% to 10% has total leucocyte count between 5000 to 10000/μl.
- Abnormal and immature WBCs are present.
- In 50% of cases, the value of uric acid is raised.
- In bone marrow examination, > 20% blast cells are present. Promyelocytes are numerous especially in M3 (acute promyelocytic leukemia). See table 883.1
- Cytochemical stains, Sudan black, and peroxidase show the positive reaction.
- Auer rods can be seen in the cytoplasm of the cells.
- Nucleated red blood cells may be seen.
- PT, PTT and Thrombin time are elevated.
- Thrombocytopenia may be present and may see the platelets count between 30,000 to 100,000/μl.
Laboratory findings in acute lymphocytic leukemia (ALL)
- Total leucocyte count is variable from low to very high.
- Anemia and thrombocytopenia
- Bone marrow:
It is difficult to find normal RBCs and WBCs.
Very few WBCs are seen.
Characteristically there are blast cells.
Sudan black and peroxidase show the negative reaction.
Auer rods are absent.
Test value for the layman
Examination of peripheral blood smear and bone marrow is advised:
- If the patient has high TLC.
- If the patient has Anemia.
- If the patient has enlarged lymph nodes.
- If the patient has weakness and fever.
References
- Bennett JM, Catovsky D, Daniel MT, et al. Proposals for the classification of the acute leukemias: French-American-British (FAB) Cooperative Group. Br J Hematol 1976;33:451-8.
- Bennett JM, Catovsky D, Daniel MT, et al. Proposed revised criteria for the classification of acute myeloid leukemia. Ann Intern Med 1985;103:620-5.
- Jaffe ES, Harris NL, Stein H, Vardiman JW (Eds). World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of Hematopoietic and Lymphoid Tissues. Lyon; IARC Press, 2001.
- Bennett JM, Catovsky D, Daniel MT, et al. Proposal for the recognition of minimally differentiated acute myeloid leukemia (AML-M0). Br J Hematol 1991; 78:325-9.
- Comment
- Posted by Dayyal Dg.