Disorders of Thyroid Gland: Hypothyroidism & Hyperthyroidism
Within the spectrum of endocrine disorders, thyroid-related conditions are prevalent and are second only to diabetes mellitus in terms of frequency. These disorders exhibit a higher incidence in females compared to males. Functional disorders of the thyroid can be bifurcated into two categories based on the gland’s activity level: hypothyroidism, characterized by a deficiency of thyroid hormones, and hyperthyroidism, marked by an overproduction of thyroid hormones. Each of these conditions can stem from a multitude of causes.
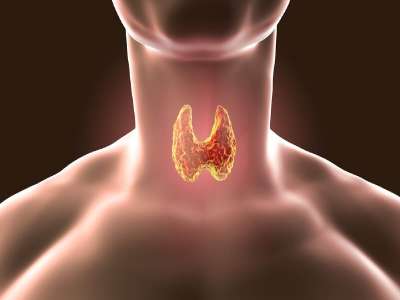
Thyroid disease encompasses a variety of conditions that affect the functionality of the thyroid gland, a crucial component of the endocrine system. This butterfly-shaped gland, nestled at the front of the neck, plays a pivotal role in regulating numerous physiological processes by synthesizing and releasing thyroid hormones, namely thyroxine (T4) and triiodothyronine (T3).
Thyroid disease also encompasses other conditions such as thyroiditis, an inflammatory condition of the thyroid gland; thyroid nodules, which are abnormal growths or lumps on the thyroid gland; goiter, a condition marked by an enlarged thyroid gland; and thyroid cancer.
The proper functioning of the thyroid is integral to the body's overall well-being. Anomalies in thyroid function can have far-reaching effects on various bodily functions, including metabolism, cognitive development, bone health, heart rate regulation, mood stability, and energy levels. Despite the challenges posed by thyroid diseases, they are typically manageable and often treatable with medication, offering a promising prognosis for those affected.
An enlargement of the thyroid gland is referred to as a goiter. The terminology associated with thyroid disorders is delineated in Box 1.
Box 1: Terminology in thyroid disorders
- Primary hyper-/hypothyroidism: Increased or decreased function of thyroid gland due to disease of thyroid itself and not due to increased or decreased levels of TRH or TSH.
- Secondary hyper-/hypothyroidism: Increased or decreased function of thyroid gland due to increased or decreased levels of TSH.
- Tertiary hypothyroidism: Decreased function of thyroid gland due to decreased function of hypothalamus.
- Subclinical thyroid disease: A condition with abnormality of thyroid hormone levels in blood but without specific clinical manifestations of thyroid disease and without any history of thyroid dysfunction or therapy.
- Subclinical hyperthyroidism: A condition with normal thyroid hormone levels but with low or undetectable TSH level.
- Subclinical hypothyroidism: A condition with normal thyroxine and triiodothyronine level along with mildly elevated TSH level.
Hyperthyroidism
Hyperthyroidism is a medical condition precipitated by the overproduction of thyroid hormone. The etiological factors contributing to hyperthyroidism encompass the following:
- Graves' disease, also known as Diffuse Toxic Goiter
- Toxic manifestations in Multinodular Goiter
- Toxicity associated with Adenoma
- Subacute Thyroiditis
- TSH-secreting Pituitary Adenoma, leading to Secondary Hyperthyroidism
- Trophoblastic tumors that secrete a TSH-like hormone, such as Choriocarcinoma and Hydatidiform Mole
- Factitious Hyperthyroidism
Clinical Characteristics
The clinical manifestations of hyperthyroidism encompass a range of symptoms including nervousness, anxiety, irritability, and insomnia, along with the presence of fine tremors. Despite maintaining a normal or even increased appetite, individuals may experience weight loss. Additional symptoms include intolerance to heat, increased perspiration, and dyspnea upon exertion. Reproductive issues such as amenorrhea and infertility may also be present. Cardiovascular symptoms can include palpitations, tachycardia, cardiac arrhythmias, and in elderly patients, heart failure. Musculoskeletal symptoms may manifest as muscle weakness, proximal myopathy, and osteoporosis, particularly in elderly individuals.
Graves' disease, a specific form of hyperthyroidism, is characterized by a triad of symptoms: hyperthyroidism itself, ophthalmopathy (manifesting as exophthalmos, lid retraction, lid lag, corneal ulceration, and impaired eye muscle function), and dermopathy, specifically pretibial myxoedema.
Box 2: Thyroid function tests in hyperthyroidism
- Thyrotoxicosis:
- Serum TSH low or undetectable
- Raised total T4 and free T4.
- T3 toxicosis:
- Serum TSH undetectable
- Normal total T4 and free T4
- Raised T3
Laboratory Features
In the majority of patients, there is an observed elevation in the levels of free serum T3 and T4. In instances of T3 thyrotoxicosis, which accounts for 5% of thyrotoxicosis cases, serum T4 levels remain within normal parameters while T3 levels are elevated. Serum TSH levels are either low or undetectable (less than 0.1 mU/L) as indicated in Box 2.
A condition known as subclinical hyperthyroidism is characterized by undetectable or low serum TSH in conjunction with normal T3 and T4 levels. This condition may present with subtle signs and symptoms of thyrotoxicosis, although this is not always the case. Subclinical hyperthyroidism carries associated risks, including atrial fibrillation, osteoporosis, and the potential progression to overt thyroid disease.
A comparative analysis of the features of primary and secondary hyperthyroidism is presented in Table 1.
| Parameter | Primary hyperthyroidism | Secondary hyperthyroidism |
|---|---|---|
| Serum TSH | Low | Normal or high |
| Serum free thyroxine | High | High |
| TSH receptor antibodies | May be positive | Negative |
| Causes | Graves’ disease, toxic multinodular goiter, toxic adenoma | Pituitary adenoma |
Evaluation of hyperthyroidism is presented in Flowchart 1.
- TSH, FT4
- Low TSH, high FT4
- Primary hyperthyroidism
- TRAb and isotope thyroid scan
- TRAb +ve, Diffuse uptake
- Graves' disease
- TRAb -ve, Nodular uptake
- Toxic adenoma
- TRAb -ve, Irregular uptake
- Toxic multinodular goiter
- TRAb +ve, Diffuse uptake
- TRAb and isotope thyroid scan
- Primary hyperthyroidism
- Low TSH, normal FT4
- Measure FT3
- Normal
- *Subclinical or mild hyperthyroidism
*Non-thyroidal illness
*Drugs (Dopamine, steroids, amiodarone)
- *Subclinical or mild hyperthyroidism
- High
- T3 thyrotoxicosis
- Normal
- Measure FT3
- High TSH, high FT4
- *Pituitary-secreting adenoma (Secondary hyerthroidism)
*Thyroid hormone resistance- TRH test
- Increased response
- Resistance to thyroid hormone
- No response
- Pituitary adenoma
- Increased response
- TRH test
- *Pituitary-secreting adenoma (Secondary hyerthroidism)
- Low TSH, high FT4
Hypothyroidism
Hypothyroidism is a condition caused by deficiency of thyroid hormones. Causes of hypothyroidism are listed below.
- Primary hypothyroidism (Increased TSH)
- Iodine deficiency
- Hashimoto’s thyroiditis
- Exogenous goitrogens
- Iatrogenic: surgery, drugs, radiation
- Secondary hypothyroidism (Low TSH): Diseases of pituitary
- Tertiary hypothyroidism (Low TSH, Low TRH): Diseases of hypothalamus
Primary hypothyroidism is characterized by an insufficiency in thyroid hormone production, which is not attributable to disorders of the hypothalamus or pituitary gland. Secondary hypothyroidism, on the other hand, arises from a deficiency in the secretion of Thyroid Stimulating Hormone (TSH) from the pituitary gland. A deficiency or loss of secretion of thyrotropin-releasing hormone from the hypothalamus results in what is known as tertiary hypothyroidism. Both secondary and tertiary hypothyroidism are significantly less common than primary hypothyroidism. Plasma TSH levels are elevated in primary hypothyroidism and reduced in secondary and tertiary hypothyroidism. The distinctions between primary and secondary hypothyroidism are delineated in Table 2.
| Parameter | Primary hypothyroidism | Secondary hypothyroidism |
|---|---|---|
| Cause | Hashimoto’s thyroiditis | Pituitary disease |
| Serum TSH | High | Low |
| Thyrotropin releasing hormone stimulation test | Exaggerated response | No response |
| Antimicrosomal antibodies | Present | Absent |
Box 3: Thyroid function tests in hypothyroidism
- Primary hypothyroidism
- Serum TSH: Increased (proportional to degree of hypofunction)
- Free T4: Decreased
- TRH stimulation test: Exaggerated response
- Secondary hypothyroidism
- Serum TSH: Decreased
- Free T4: Decreased
- TRH stimulation test: Absent response
- Tertiary hypothyroidism
- Serum TSH: Decreased
- FT4: Decreased
- TRH stimulation test: Delayed response
The clinical manifestations of primary hypothyroidism include lethargy, mild depression, menstrual irregularities, weight gain, intolerance to cold, dry skin, myopathy, constipation, and a firm and lobulated thyroid gland, a characteristic feature of Hashimoto’s thyroiditis.
In severe instances, a condition known as myxoedema coma may occur. This advanced stage is marked by stupor, hypoventilation, and hypothermia.
Laboratory Indicators
The laboratory indicators associated with hypothyroidism are detailed in Box 3.
A condition known as subclinical hypothyroidism is characterized by normal serum thyroxine (T4 and FT4) levels in conjunction with a moderately elevated TSH level (greater than 10 mU/L). This condition is associated with adverse obstetrical outcomes, impaired cognitive development in children, and an increased risk of hypercholesterolemia and progression to overt hypothyroidism.
The evaluation process for hypothyroidism is depicted in Flowchart 2.
- TSH, FT4
- High TSH, low FT4
- Primary hypothyroidism
- Thyroid microsomal antibody
- Increased
- Hashimoto's thyroiditis
- Normal
- *Congenital T4 synthesis deficiency
*Iodine deficiency
- *Congenital T4 synthesis deficiency
- Increased
- Thyroid microsomal antibody
- Primary hypothyroidism
- High TSH, normal FT4
- Subclinical hypothyroidism
- Low TSH, low FT4
- Secondary or tertiary hypothyroidism
- TRH stimulation test
- Little or no TSH response
- Secondary (Pituatary) hypothyroidism
- Delayed TSH response
- Tertiary (Hypothalamic) hypothyroidism
- Little or no TSH response
- TRH stimulation test
- Secondary or tertiary hypothyroidism
- High TSH, low FT4
References
- Demers LM. Thyroid disease: pathophysiology and diagnosis. Clin Lab Med 2004;24:19-28.
- Heuck CC, Kallner A, Kanagasabapathy AS, Riesen W. Diagnosis and monitoring of diseases of thyroid. World Health Organization. 2000 WHO/DIL/0.004.
- Kaplan MM. Clinical perspectives in the diagnosis of thyroid disease. Clin Chem 1999;45:1377-83
- Lazarus JH, Obuobie K. Thyroid disorders—an update. Postgrad Med J 2000;76:529-36.
- Comment
- Posted by Dayyal Dg.