Antibiotic resistance is a curse to the present world
Antibiotics saved thousands of people in 1950s and 1960s. But for decades these antibiotics show lower efficacy against microbial infections. Antibiotic resistance is now one of the most concerning issues in the present world. It is suspected that we are turning back into the pre-antibiotic era, in which no effective antibiotic is available.
Every year, multidrug-resistant bacteria causes death to 25,000 patients in the EU. Hospital-acquired bacterial infections kill 63,000 patients in the United States each year. This increased resistance may kill 10 million people by 2050.
Bacteria become resistant to antibiotics by various mechanisms. There are a lot of mechanisms of antibiotic resistance.
These mechanisms include the production of beta-lactamase that destroys antibiotics, changes in the bacterial cell wall, production of efflux pumps and altering the metabolic pathways.
It is very essential to combat antimicrobial resistance. We should first prevent antimicrobial resistance or control it, develop a new antimicrobial drug.
There are a number of antibiotic alternatives. Research should be focused on these alternatives to prevent or control antibiotic resistance and microbial infection.
Why is the end of the antibiotic era possible?
As antibiotic resistance is increasing day by day, most effective antibiotics become ineffective.
Several antibiotics were the last choice of antibiotic-resistant bacteria. For example, vancomycin was used against Gram-positive bacteria and carbapenems against Gram-negative bacteria. These antibiotics lost their efficacy against these bacteria.
Are we turning back toward the pre-antibiotic era in which no effective antibiotics are available?
Because of this increased resistance, there is a possibility to go back in the pre-antibiotic era. There are several reasons.
1. In 1941, Albert Alexander was treated with an antibiotic as a first patient of history. Since then two human generations have passed. But more than 46,000 bacterial generations have passed. Because one generation of bacteria ends within 20 minutes. So there is a good chance to occur a remarkable microbial evolution. These evolutions cause bacterial resistance to antibiotics.
2. Since 1941 human and animal consumed a large number of antibiotics. On average, a child under the age of 18 years consumes ten to twenty courses of antibiotics. Physicians prescribed 160 million prescriptions for antibiotics. These prescriptions estimate approximately 25,000 tons of antibiotics.
Half of this amount is consumed by human. Other half is used for the non-human purpose such as animal husbandry, agriculture, and aquaculture. Antibiotic resistance resulted from non- human purpose also cause serious problems. This offers several human diseases by bacteria.
3. Our body contains 1013 to 1014 bacteria. These bacterial cells are 10 times higher than our normal body cells. There are also 100 times higher bacterial genes than human genes in our body.
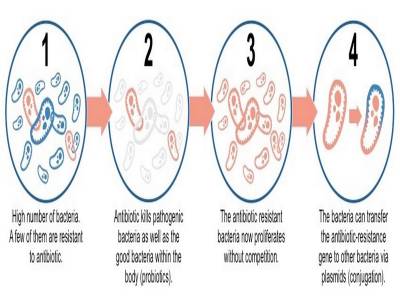
When the antibiotics enter the body it kills the susceptible bacteria. Thus it allows resistant bacteria to survive. Then it becomes very difficult to treat infection of surviving resistant bacteria in the same body. These resistant bacteria also disperse in the environment and infect other healthy people.
Excessive use of antibiotics causes a change in the gut microbiome. The gut microbiome is a major part of human bacterial flora. This changes in gut microbiome cause dysbiosis. Dysbiosis cause several gut health problems. These include leaky gut syndrome, chronic diarrhea, gas problem, and constipation.
4. There are approximately 1034 bacteria in the world. Antibiotics or antibiotic waste are discharged in the environment. These reduce the bacterial population and makes other bacteria resistant to antibiotics. This led us to an era, in which no effective antibiotics are available.
The present situation of antibiotics:
In 2013, the Centers for Disease Control & Prevention (CDC) published a report on antimicrobial resistance. They showed that antibiotic-resistant bacteria infect 2 million people and cause death to 23000 people of them every year.
In 2014 WHO published another report on antibiotic resistance. They collected this data from 114 countries. They said that antibiotic resistance is not a topic for the future. It is happening throughout the world at the present time.
Several examples of antibiotic resistance:
- Third-generation cephalosporins can no longer treat gonorrhea. This failure of antibiotic resistance leads to infertility, adverse pregnancy, and neonatal blindness.
- Fluoroquinolones have failed to treat E. coli infection and tuberculosis.
- Artemisinin can’t kill Plasmodium falciparum. This parasite causes malaria.
- Antiviral drugs used for influenza virus becomes ineffective day by day. Two antiviral drugs can’t work against influenza virus. These drugs include amantadine and rimantadine
WHY DON’T WE DEVELOP MORE ANTIBIOTICS?
If the bacteria become resistant to all antibiotics, why don’t we develop new antibiotics?
There are several reasons not to discover more antibiotics:
Scientific cause:
Many bacterial strains have become resistant to all known antibiotics. They are either extensively drug-resistant (XDR) or even pan-drug resistant (PDR) strains.
Scientists have discovered most of the commonly found antimicrobial drug already. So it is very difficult to find a new drug when they are screening for the drug. Moreover, in some cases, the potential new antimicrobial drug can't be chosen due to their higher toxicity.
Economic causes for producers:
Pharmaceutical companies lose the courage to invest money in antibiotic research. Because patients take antibiotics for a short period of time. This doesn’t create enough profit for pharmaceutical companies.
Moreover, companies have to make a license for each drug. This makes them invest more money to get licensed. There is also a risk to be rejected by the FDA.
- Comment
- Posted by Md. Jahangir Alam